Understanding Congenital Toxoplasmosis
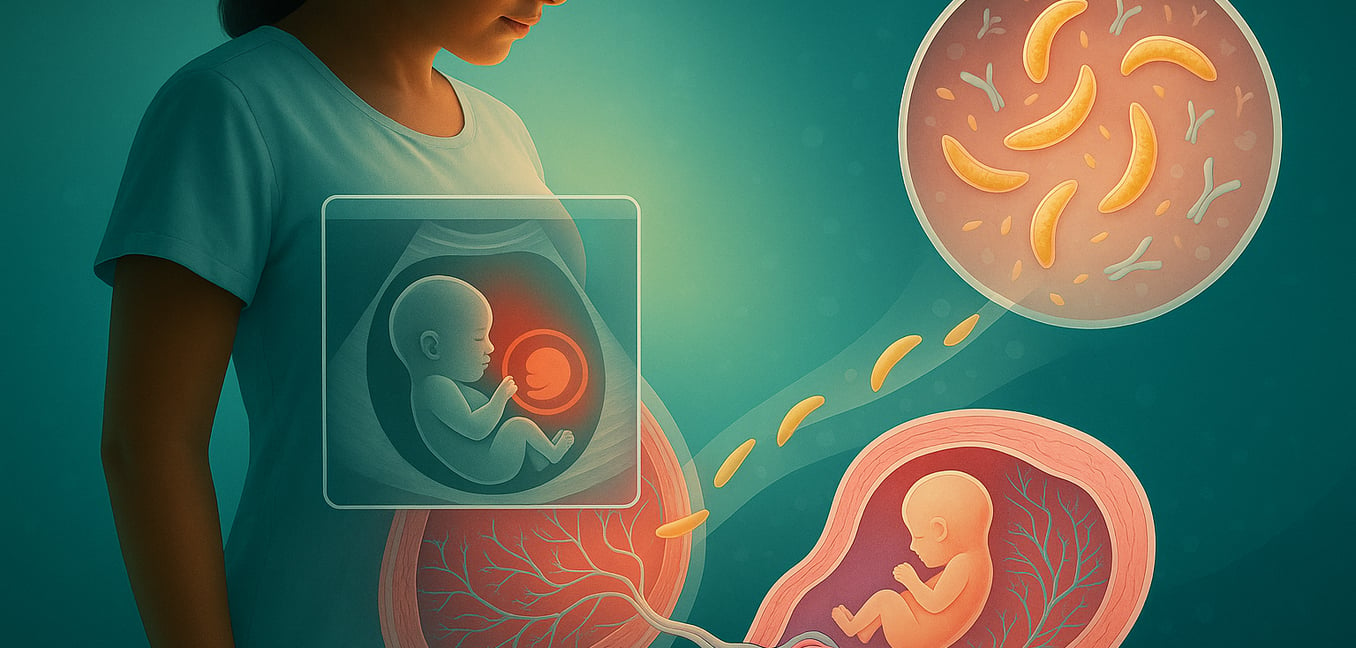
Congenital toxoplasmosis occurs when the Toxoplasma gondii parasite passes from a mother to her baby during pregnancy. This transmission typically happens when the mother contracts the infection for the first time shortly before or during pregnancy, as she lacks the immunity to control the parasite. The infection is most often acquired by eating undercooked meat containing parasite cysts or by consuming food or water contaminated with oocysts from cat feces.
The impact on the baby depends on several factors:
- Timing of Infection: The timing of the mother's infection is paradoxical. An infection early in pregnancy has a lower chance of crossing the placenta, but if it does, the consequences for the fetus are often severe, leading to major organ damage. Conversely, an infection later in pregnancy is much more likely to be transmitted, but the disease in the newborn is often less severe or even asymptomatic at birth.
- Mechanism of Harm: The parasite travels through the mother's bloodstream, crosses the placenta, and invades the fetus. It often attacks the developing brain and eyes, where the fetal immune system is naturally less active, allowing the parasite to multiply freely. This can cause inflammation, destroy tissue, and lead to serious problems like brain calcifications or excess fluid on the brain (hydrocephalus).
- Clinical Presentation: The effects of congenital toxoplasmosis range from devastating to silent. While some infants are born with severe signs like eye inflammation (chorioretinitis), hydrocephalus, and brain calcifications, the vast majority—up to 85%—appear healthy at birth. This asymptomatic presentation is deceptive, as these children risk developing long-term complications, most commonly vision problems, if the infection is not diagnosed and treated.
Prenatal Diagnosis: Detecting Infection in Utero
If a pregnant person acquires toxoplasmosis, the next critical step is determining if the parasite has crossed the placenta. Specialized prenatal testing is essential to guide treatment decisions for both mother and baby.
Key diagnostic methods include:
- Amniotic Fluid PCR Test: This molecular test detects the parasite's DNA in amniotic fluid obtained via amniocentesis, typically after 18 weeks of gestation. It provides direct proof of infection, though its accuracy depends on correct timing.
- Fetal Ultrasound: High-resolution scans check for physical signs like brain calcifications, excess fluid (hydrocephalus), or an enlarged liver and spleen. However, many infected fetuses appear normal on ultrasound, so a clear scan cannot rule out infection.
- Strategic Timing: Amniocentesis is usually performed at least four weeks after the mother's suspected infection. This delay allows the parasite enough time to reach detectable levels in the amniotic fluid, helping to prevent false-negative results that could delay necessary treatment.
Serological Testing in Newborns
After birth, diagnosis shifts to confirming infection in the newborn through blood tests (serology) that detect antibodies against the Toxoplasma parasite. The primary challenge is distinguishing between the baby's own antibodies and those that passed from the mother across the placenta.
A definitive diagnosis relies on interpreting a combination of tests over time:
- Tracking IgG Antibodies: A newborn's blood contains the mother's IgG antibodies. If these levels do not decline and disappear by 12 months, or if they begin to rise, it indicates the baby is producing their own in response to an infection.
- Detecting IgM Antibodies: These antibodies do not cross the placenta, so their presence in a newborn is strong evidence of infection. However, many infected infants do not produce detectable IgM, so a negative test is not conclusive.
- Comprehensive Antibody Profiling: Specialized labs can compare the baby's complete antibody profile to the mother's. This detailed comparison helps confirm a distinct immune response in the infant, providing the most reliable diagnosis to guide the year-long treatment plan.
The Role of Imaging and Clinical Examination
A positive or inconclusive serology result is not the end of the diagnostic journey. To understand the infection's true impact, doctors perform a complete clinical evaluation, including detailed imaging of the brain and eyes.
Comprehensive Eye Examination
A detailed eye exam by an ophthalmologist is a top priority, as the eyes are most commonly affected. Doctors look for chorioretinitis—inflammation of the retina and choroid that can cause scarring and permanent vision loss. They also check for other issues like abnormally small eyes (microphthalmia), cataracts, or damage to the macula, which is responsible for sharp, central vision.
Brain Imaging
Specialized brain imaging helps assess the central nervous system. Cranial ultrasound, CT, or MRI scans are used to find signs like hydrocephalus (fluid buildup) or intracranial calcifications (small calcium deposits). These findings often signal more severe disease and help predict long-term neurological risks, such as seizures or developmental delays.
Broader Clinical Assessment
The evaluation also includes hearing tests, as hearing loss can develop later in childhood. Doctors check for an enlarged liver or spleen, jaundice, and skin rashes. A lumbar puncture may be performed to analyze the cerebrospinal fluid for signs of inflammation, helping to create a complete health profile for the child.
Emerging Biomarkers and Advanced Diagnostic Approaches
Given the limitations of traditional antibody tests, scientists are developing new methods that focus on the body's immediate cellular immune response. These advanced tools aim to identify unique immunological "fingerprints" of the infection for a faster, more definitive diagnosis.
Measuring Inflammatory Signals
New tests can measure specific inflammatory messengers, known as chemokines, in an infant's blood. The levels of these proteins are significantly elevated in babies with congenital toxoplasmosis, acting as an alarm signal sent out by the immune system. This method can accurately distinguish infected infants from uninfected ones.
Tracking Immune Cell Activity
Instead of just looking for antibodies, other new tests track the immune system's direct response. One method measures the activity of specific immune "fighter" cells that multiply when an infection is present. Combining this with tests for inflammatory signals in the blood can confirm an infection with very high accuracy.
Assessing the Immune System's Memory
A highly promising technique involves exposing a small blood sample to Toxoplasma proteins in a lab. In infected infants, T-cells that "remember" the parasite will respond by producing a substance called interferon-gamma. Measuring this response is an extremely sensitive and accurate way to confirm an infection early in life.
Predicting Clinical Risk
Beyond diagnosis, these biomarkers can help predict an infant's risk of developing eye disease. By measuring the production of specific molecules from different immune cells, doctors can gain early insight into which babies are likely to develop retinal lesions. This helps differentiate between active, inflammatory eye disease and older, inactive scars, allowing for more tailored treatment.