Understanding Macular Corneal Dystrophy
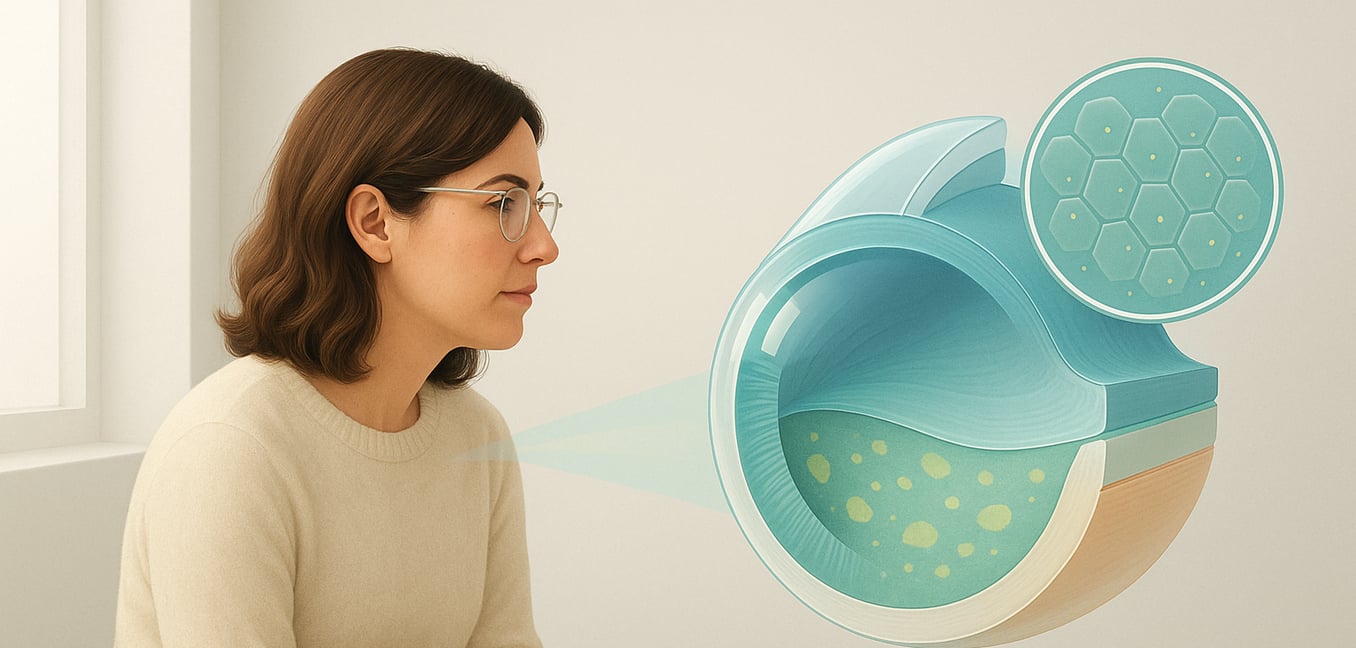
Macular corneal dystrophy is a genetic condition that causes the slow, progressive clouding of the cornea, the clear front window of the eye. It results from a faulty gene that prevents the cornea from properly processing certain materials. This leads to the buildup of abnormal sugar-like substances (known as glycosaminoglycans) within the corneal tissue, which gradually impairs vision. The condition often begins in childhood and worsens over decades, requiring a treatment approach that evolves with the disease.
Initially, the focus is on managing symptoms like pain and light sensitivity with non-surgical options. As the clouding worsens and significantly affects sight, surgery becomes necessary to restore vision by addressing the diseased corneal tissue. Long-term management then centers on monitoring the health of the eye and managing any potential return of the condition.
Non-Surgical Options for Symptom Management
While surgery is the ultimate solution for restoring vision, non-surgical strategies can effectively manage symptoms in the earlier stages. These treatments aim to enhance daily comfort, protect the eye’s surface, and preserve vision for as long as possible.
- Medicated Eye Drops and Ointments: Lubricating drops soothe dryness and a gritty sensation. Hypertonic saline solutions (e.g., 5% sodium chloride) are specialized salt-based drops or ointments that draw excess fluid from the cornea, helping to reduce swelling and improve vision.
- Therapeutic Bandage Contact Lenses: For painful recurrent corneal erosions, where the cornea's surface breaks down, a special soft contact lens can act as a protective shield. It covers exposed nerve endings to reduce pain and creates a stable environment for the cornea to heal underneath.
- Corrective Eyeglasses and Contacts: While glasses cannot clear the corneal clouding, they are essential for correcting focusing problems like astigmatism that are caused or worsened by the dystrophy. In some cases, specialized scleral lenses can provide superior vision by creating a smooth optical surface over the irregular cornea.
Surgical Treatments to Restore Vision
When vision becomes significantly impaired, surgery offers a highly effective way to restore sight. The goal is to remove the cloudy, diseased corneal tissue and, if necessary, replace it with a clear, healthy cornea from a donor. Modern techniques allow surgeons to tailor the procedure to the patient's specific needs.
- Phototherapeutic Keratectomy (PTK): This laser procedure removes microscopic layers from the cornea's surface. It is most effective when cloudy deposits are shallow, as it can clear the visual axis without needing donor tissue. However, since macular dystrophy often involves deep clouding, PTK may only offer temporary improvement.
- Deep Anterior Lamellar Keratoplasty (DALK): As a preferred partial-thickness transplant, DALK involves removing the diseased outer and middle layers of the cornea while leaving the patient’s own healthy innermost layer (the endothelium). This technique lowers the risk of graft rejection and leads to a stronger eye with faster visual recovery.
- Penetrating Keratoplasty (PK): This traditional full-thickness transplant replaces the entire central portion of the cloudy cornea with a donor cornea. While highly effective, PK is more invasive than DALK and carries a higher lifelong risk of graft rejection. It is typically reserved for cases where the clouding is extremely dense or a DALK procedure is not possible.
Following surgery, the prognosis for vision is very good. However, because the underlying genetic issue remains, the cloudy deposits can slowly return on the new graft over many years, a problem known as recurrence.
The Future of Treatment: Gene Therapy and Research
Current treatments are excellent for restoring vision, but they don't fix the root genetic cause of macular corneal dystrophy, leading to the possibility of recurrence. This has driven research into therapies that aim to provide a permanent cure.
- Gene Replacement Therapy: This approach would introduce a healthy copy of the defective CHST6 gene into corneal cells. By enabling the cells to produce the correct enzyme, it could permanently halt the cloudy buildup and prevent the disease from returning.
- Enzyme Replacement Therapy (ERT): An alternative strategy is to supply the missing enzyme directly to the cornea, possibly through specialized eye drops. This would help cells process materials correctly, clearing existing deposits and preventing new ones, though it would likely require ongoing treatment.
- Gene Editing: Using powerful tools like CRISPR-Cas9, scientists hope to one day directly repair the patient’s own defective gene within their corneal cells. This would offer a one-time, permanent cure by restoring the cornea's natural function and completely eliminating the disease.