The Genetics of Corneal Dystrophy: A Guide to Risk Factors
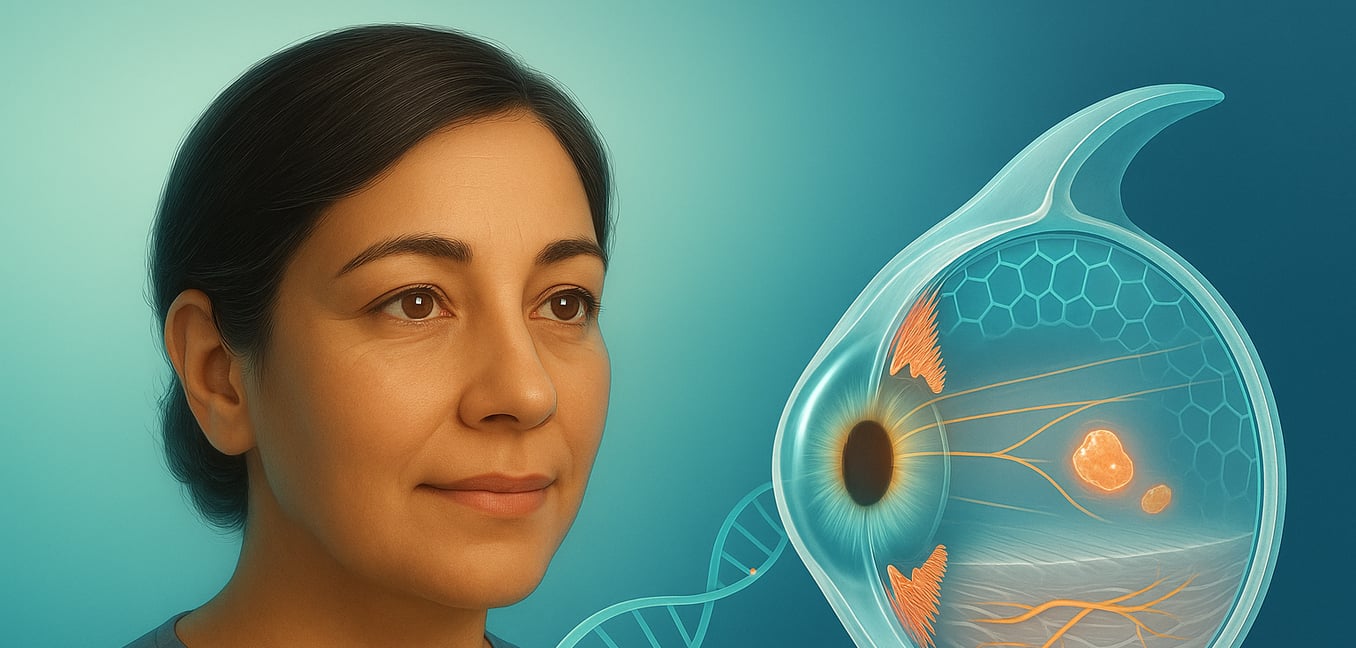
The cornea is the clear, protective outer layer of your eye. Like a camera lens, it focuses light to help you see. Corneal dystrophies are a family of genetic disorders that cause abnormal material to build up in the cornea, making it cloudy and impairing vision over time.
These conditions are defined by a few key traits. They are inherited, passed down through families due to specific flaws in a person's genetic code. They are not caused by injury, infection, or lifestyle factors. These disorders typically affect both eyes, though not always symmetrically, and they tend to be progressive, meaning symptoms worsen slowly over many years or decades.
At the heart of every dystrophy is a genetic mistake that disrupts the normal function of corneal cells. This causes the cells to produce or accumulate substances, such as proteins or fats, that they cannot properly clear. This buildup creates cloudiness or irregularities in the corneal tissue, leading to symptoms like blurred vision, glare, light sensitivity, and sometimes pain. The most common inheritance pattern is autosomal dominant, where a single copy of the mutated gene from one parent is enough to cause the condition, giving each child of an affected parent a 50% chance of inheriting it.
The TGFBI Gene: A Common Culprit
While many genes can cause corneal dystrophies, a single gene—Transforming Growth Factor, Beta-Induced (TGFBI)—is responsible for several of the most common types.
The TGFBI gene provides instructions for making a protein called keratoepithelin. In a healthy eye, this protein helps maintain the cornea's structure and transparency. However, when the TGFBI gene is mutated, it produces a faulty version of this protein. This abnormal protein misfolds and clumps together, forming deposits within the cornea that disrupt vision.
Remarkably, different mutations within this one gene can cause several distinct dystrophies, each with a unique appearance. The specific type of mutation determines how the protein clumps, creating deposits that may look like crumbs (Granular Dystrophy), branching lines (Lattice Dystrophy), or other patterns an ophthalmologist can see during an exam. These TGFBI-related dystrophies are almost always inherited in an autosomal dominant pattern.
Genetic Factors in Epithelial and Stromal Dystrophies
Dystrophies affecting the cornea's outer (epithelial) and middle (stromal) layers are caused by a diverse range of genetic mutations. These flaws disrupt everything from the cornea's structural integrity to its chemical balance.
Meesmann Dystrophy This condition is caused by mutations in the KRT3 and KRT12 genes. These genes produce keratin, a protein that provides structural strength to the cornea's outer cells. When these genes are faulty, the outer layer becomes fragile, leading to the formation of tiny cysts that can cause irritation and blurred vision.
Macular Dystrophy Linked to mutations in the CHST6 gene, this is one of the most visually significant stromal dystrophies. Unlike the dominant TGFBI dystrophies, Macular Dystrophy is autosomal recessive, meaning a person must inherit a defective gene from both parents. The mutation disrupts the processing of a molecule called keratan sulfate, causing a widespread, milky haze to form across the cornea, often leading to severe vision loss.
Lattice Dystrophy Type 2 (Meretoja Syndrome) While most lattice dystrophies are caused by TGFBI mutations, this specific type is caused by a defect in the gelsolin (GSN) gene. The faulty gelsolin protein forms amyloid deposits in the cornea, but the condition is also systemic. This means the amyloid builds up in other body tissues, causing problems like sagging skin and nerve issues, making the eye findings a clue to a broader health condition.
Genetic Insights into Endothelial Dystrophies
The endothelium, the cornea's innermost layer, is a pump that removes fluid to maintain clarity. When the genes governing these cells are flawed, the pump fails, causing the cornea to swell and vision to become hazy.
Fuchs' Endothelial Corneal Dystrophy (FECD) The most common endothelial dystrophy, FECD has different genetic causes based on its onset.
- Late-Onset FECD: Most often caused by a flaw in the TCF4 gene where a small piece of DNA code repeats too many times. These excessive repeats create toxic material that clogs the cell's machinery, causing it to die off slowly.
- Early-Onset FECD: This rarer form is usually linked to mutations in the COL8A2 gene. This gene helps build the foundation that endothelial cells rest on. A faulty gene creates a weak base, leading to premature cell failure.
Posterior Polymorphous Corneal Dystrophy (PPCD) This condition results from mutations in "master switch" genes like ZEB1. These genes tell endothelial cells how to behave. When mutated, the instructions get scrambled, causing the cells to grow in abnormal layers and disrupt the cornea's architecture, sometimes leading to secondary glaucoma.
Congenital Hereditary Endothelial Dystrophy (CHED) This severe, recessive condition is linked to the SLC4A11 gene. This gene builds a crucial transporter protein that helps regulate fluid. When a child inherits two faulty copies, the transporter fails, causing the endothelial pump to be dysfunctional from birth and leading to immediate, persistent corneal clouding.
The State of Genetic Discovery: The IC3D Classification
As genetic discoveries advance, scientists need a system to organize this knowledge. To address this, the International Classification of Corneal Dystrophies (IC3D) was developed. This system groups dystrophies into four categories based on how well the genetic cause is understood.
- Category 1: Reserved for dystrophies where the specific gene causing the condition has been identified and confirmed. This includes well-established conditions like the TGFBI-related dystrophies and Meesmann dystrophy.
- Category 2: Includes dystrophies that have been mapped to a specific location on a chromosome, but the exact gene has not yet been identified. Researchers know the genetic "address" but haven't found the specific "house."
- Category 3: For dystrophies that are clinically well-defined and known to be hereditary, but for which no specific gene or chromosomal location has been found. The underlying genetic cause remains a mystery.
- Category 4: A holding category for newly discovered or suspected dystrophies that are not yet well-defined. As more is learned, these conditions may be moved to another category or established as a new disease.