Understanding Recessive X-Linked Ichthyosis: A Brief Overview
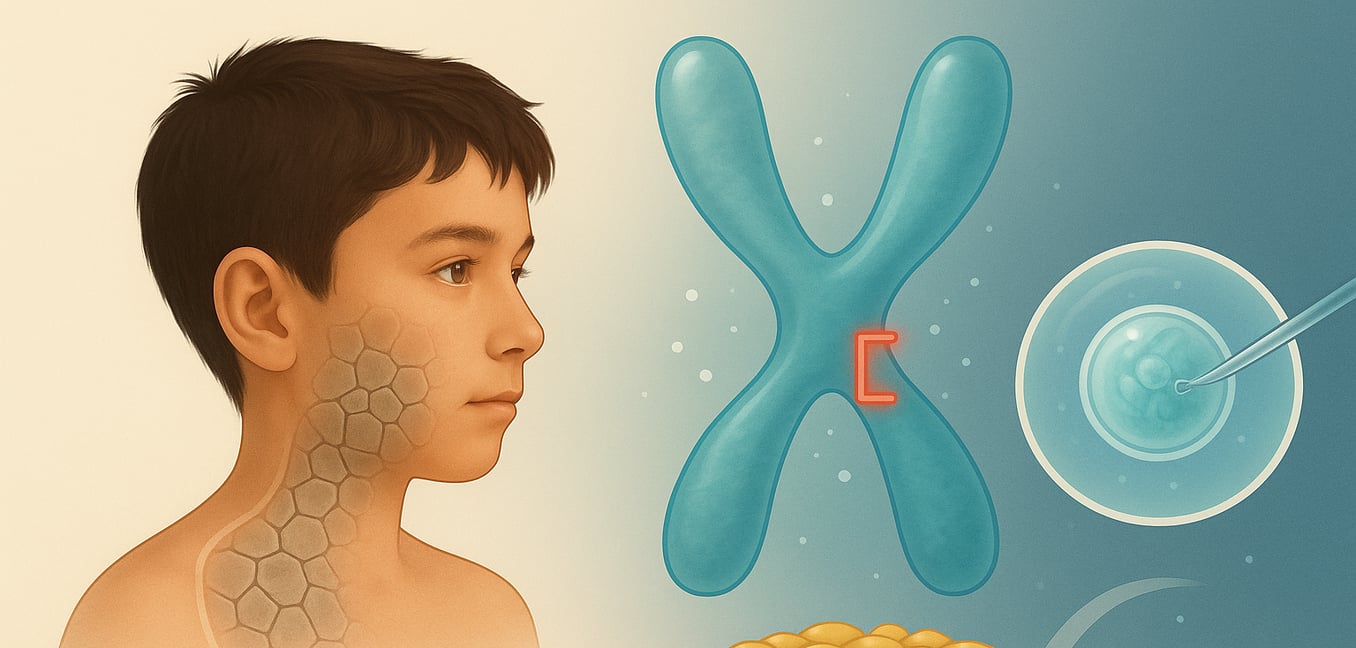
Recessive X-linked ichthyosis (RXLI) is a genetic skin condition that primarily affects males. Also known as steroid sulfatase (STS) deficiency, it disrupts the skin's natural shedding cycle. While the body produces new skin cells normally, the old ones do not shed properly, leading to an accumulation on the skin's surface.
This buildup causes the primary symptom: dry, scaly skin. The scales are often large, dark, and polygonal, sometimes creating a "dirty" appearance, especially on the neck and trunk[^1[^3]3]. Symptoms typically appear within the first few months of life and can worsen in cold, dry weather. The palms, soles, and flexural areas like the inner elbows are usually spared.
The condition is caused by a deletion or mutation in the STS gene on the X chromosome. This gene provides instructions for making the steroid sulfatase enzyme. Without this enzyme, a substance called cholesterol sulfate accumulates in the skin. This buildup strengthens the bonds between skin cells, which blocks the natural skin-shedding process and weakens the skin's protective barrier.
The First Step: The Role of Genetic Counseling
For families impacted by RXLI, genetic counseling is an essential first step in understanding and managing risk. A genetic counselor is a trained professional who translates complex genetic information into practical, understandable terms, creating a supportive space for you to make informed decisions.
Clarifying Family Risk
A counselor will help you map out your family's medical history to see how the condition is passed down. They explain the specifics of X-linked recessive inheritance, clarifying why males are primarily affected while females can be carriers, often without symptoms. This process provides personalized risk assessments, such as the 50% chance that a carrier mother will pass the condition to a son.
Exploring Your Options
The counselor provides a comprehensive overview of available genetic testing pathways. They will discuss the purpose of different tests, such as carrier screening for female relatives or diagnostic testing during pregnancy[^12]. This conversation covers the benefits and small risks associated with each option, ensuring you have the information you need to choose a path forward.
Providing Support and Resources
Receiving a diagnosis or learning about carrier status can be an emotional experience. Counselors are trained to help families process this information in a supportive, non-judgmental environment. They also serve as a bridge to other resources, connecting you with patient advocacy groups, online communities, and medical specialists who can offer ongoing support.
Confirming Risk: Genetic Testing and Diagnosis
A definitive diagnosis is key to prevention and management. This can happen before or after birth, using specific tests to identify the underlying genetic cause.
Initial Clues During Pregnancy
Sometimes, the first indication of RXLI appears during routine prenatal screening. Unusually low levels of the hormone estriol in a mother's blood can be a red flag. The placenta needs the STS enzyme from the fetus to produce estriol, so low levels may suggest STS deficiency. While not conclusive on its own, this finding typically prompts a recommendation for further diagnostic testing.
Definitive Diagnosis Before Birth
For families with a known history of RXLI or following an abnormal screening result, prenatal diagnostic tests can confirm if a fetus is affected. These procedures obtain a sample of the fetus's genetic material for analysis.
- Chorionic Villus Sampling (CVS): Typically performed between 10 and 13 weeks of pregnancy, this test involves taking a small sample of tissue from the placenta.
- Amniocentesis: Usually done between 15 and 20 weeks, this procedure involves collecting a small amount of amniotic fluid surrounding the fetus.
DNA from either sample is then analyzed in a lab to look for the deletion or mutation of the STS gene, providing a clear diagnosis.
Diagnosis After Birth
RXLI is often diagnosed in infancy when a baby develops the characteristic large, dark scales. A simple blood test is used to analyze the baby's DNA and confirm the absence or mutation of the STS gene. This genetic confirmation is vital to distinguish RXLI from other types of ichthyosis and establish the right management plan.
Identifying Carriers in the Family
After a male is diagnosed, his female relatives can choose to learn their carrier status through a blood test that analyzes their DNA for the same STS gene mutation. Knowing this information can empower a woman to understand her own health and make informed decisions about future family planning.
Proactive Prevention: Advanced Family Planning Strategies
For families aware of their risk for RXLI, advanced medical technologies offer pathways for proactive family planning, allowing parents to navigate their reproductive journey with greater certainty.
Prenatal Diagnosis for Preparation and Decision-Making
As described previously, prenatal tests like CVS and amniocentesis can determine if a fetus has inherited RXLI. This definitive knowledge, obtained early in pregnancy, is powerful. It allows parents to prepare emotionally and logistically for a child with specific medical needs and to arrange for specialized care. It also empowers them to make deeply personal decisions regarding the continuation of the pregnancy, supported by comprehensive genetic counseling that honors the family's values.
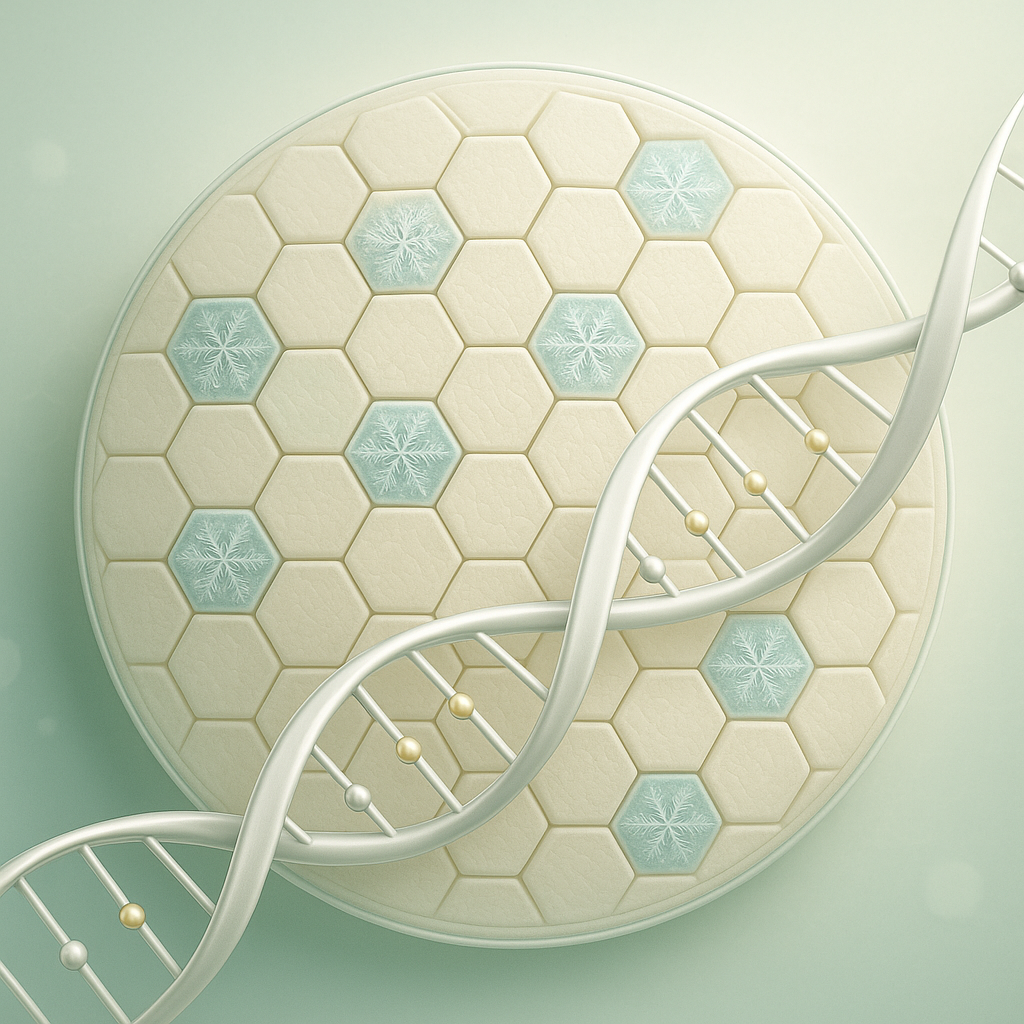
Preimplantation Genetic Diagnosis for Prevention
Preimplantation genetic diagnosis (PGD) offers a different approach by screening for RXLI before a pregnancy begins. This technology is used in conjunction with in vitro fertilization (IVF).
- Embryos are created in a laboratory.
- Before an embryo is transferred to the uterus, a few cells are carefully tested for the STS gene mutation.
- Only embryos found to be unaffected by the condition are selected for implantation.
This process gives parents a very high degree of confidence that their child will not inherit the disorder. For many families, PGD is a preferred route as it avoids the difficult decisions that can arise from a diagnosis made later in pregnancy.