Understanding Glutaryl-CoA Dehydrogenase Deficiency: The Basis for Prevention
Glutaric Acidemia Type 1 (GA1) is an inherited disorder caused by a faulty enzyme, glutaryl-CoA dehydrogenase (GCDH). This condition prevents the body from correctly processing certain amino acids—lysine, hydroxylysine, and tryptophan—which are essential building blocks of proteins. To understand how GA1 can be managed and its severe effects prevented, it's crucial to grasp the following key aspects:
- The GCDH Enzyme's Job: Think of the GCDH enzyme as a specialized worker in the body's metabolic factory. Its primary task is to help break down lysine, hydroxylysine, and tryptophan into forms the body can use for energy or other vital functions. When a genetic mutation causes this enzyme to malfunction, this critical processing step is blocked.
- Consequences of Enzyme Failure: Without a working GCDH enzyme, the intermediate products from lysine, hydroxylysine, and tryptophan metabolism—such as glutaric acid, glutaryl-CoA, and 3-hydroxyglutaric acid—begin to accumulate. These substances are not meant to be present in high concentrations and can become toxic, particularly to brain tissue.
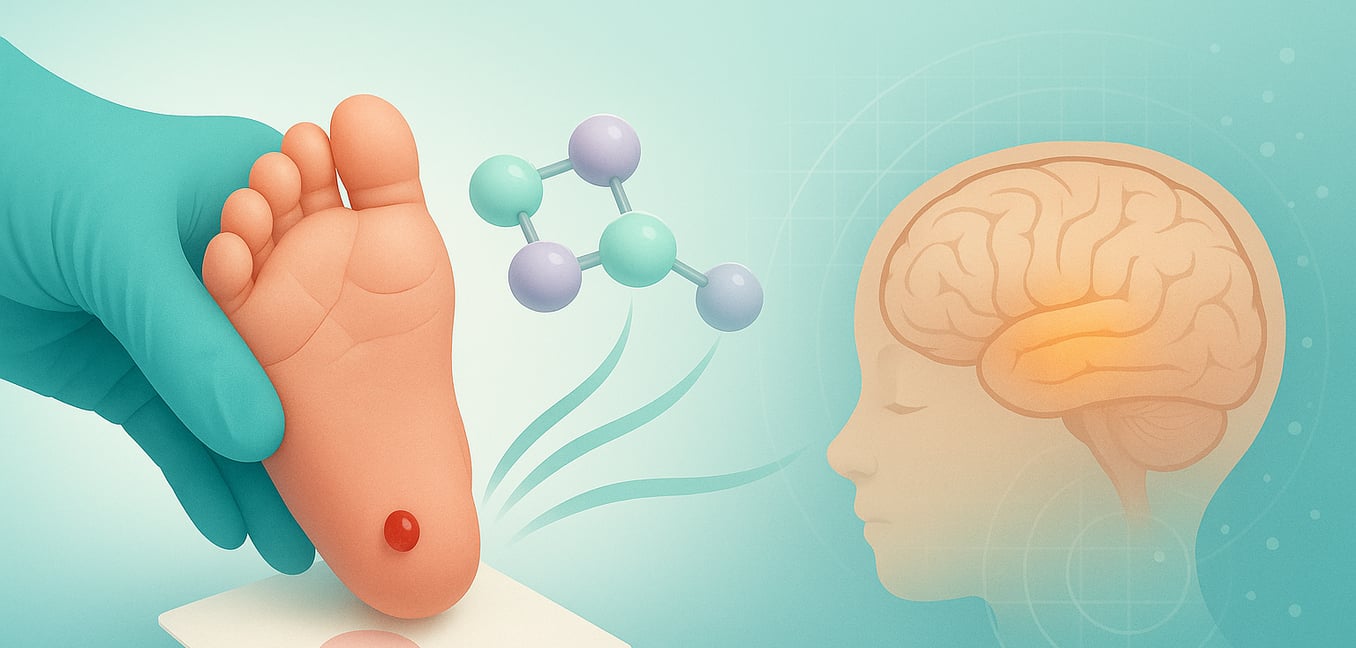
- Brain Vulnerability, Especially the Basal Ganglia: The brain is highly susceptible to these accumulating toxins. A specific area, the basal ganglia, which plays a vital role in controlling movement and learning, often sustains significant damage. This toxic buildup can lead to acute injury in this region (striatal necrosis), resulting in the characteristic movement disorders, spasms, and rigidity seen in GA1.
- Secondary Carnitine Depletion: The body attempts to detoxify and remove these harmful organic acids by using carnitine. Carnitine binds to these acids, forming compounds like glutarylcarnitine, which are more easily excreted. However, the constant high levels of these acids in GA1 can deplete the body's carnitine reserves, leading to a secondary carnitine deficiency. This can worsen muscle weakness and further hinder detoxification.
The Critical Role of Newborn Screening in Early Detection
Identifying Glutaric Acidemia Type 1 (GA1) at the earliest possible stage is paramount, particularly because affected infants often appear healthy at birth. Newborn screening serves as an essential early warning system, providing a vital opportunity to intervene before the disorder inflicts serious, often irreversible, neurological damage. This proactive strategy is fundamental to prevention.
The effectiveness of newborn screening for GA1 is based on several key factors:
- Efficient Screening Process: Newborns are typically screened within a day or two of birth using a simple heel prick. A few drops of blood collected on filter paper are sent to a laboratory for analysis with a technique called tandem mass spectrometry. This technology detects abnormal levels of specific substances; for GA1, elevated glutarylcarnitine (C5DC) is a key indicator. A positive initial screen prompts further confirmatory tests, like urine organic acid analysis and genetic testing.
- Preventing Acute Neurological Damage: The foremost benefit of early detection is initiating treatment before an acute encephalopathic crisis—a sudden neurological decline often triggered by illness or metabolic stress. Such crises can cause severe, permanent brain damage, especially to the basal ganglia. By identifying GA1 in asymptomatic newborns, preventative measures can drastically reduce this risk, preserving brain function and improving long-term outcomes.
- Timely Management Strategies: An early diagnosis allows for the immediate start of crucial management. This includes a special diet low in lysine and tryptophan to reduce toxic metabolite production. Carnitine supplementation is also initiated to aid detoxification and address secondary deficiency. Families receive education on emergency protocols for managing intercurrent illnesses.
- Continuous Program Improvement: Newborn screening programs strive to enhance detection, especially for "low excretors" who may have only mildly elevated biochemical markers. Ongoing research focuses on refining screening algorithms, potentially using marker ratios or second-tier tests, to improve sensitivity and ensure more affected infants benefit from early intervention.
Dietary Interventions: Managing Lysine and Tryptophan Intake
Careful dietary management is a cornerstone of preventing complications in GA1. Since the body cannot properly break down the amino acids lysine and tryptophan, controlling their intake is crucial to stop the buildup of harmful substances that can damage the brain.
This specialized dietary approach involves several key strategies:
- Strict Lysine Restriction: Significantly reducing lysine intake is a primary goal and is strongly linked to better long-term outcomes, especially if started early after newborn screening. This is achieved using specialized medical formulas very low in lysine and by limiting natural foods rich in this amino acid (e.g., meat, dairy, eggs). The aim is to provide only the minimal lysine needed for growth, avoiding excess.
- Balanced Tryptophan Management: Tryptophan intake also requires careful control. While it's a precursor to harmful metabolites in GA1, tryptophan is also essential for producing serotonin, a vital neurotransmitter. Medical formulas are designed to restrict tryptophan but not eliminate it, ensuring enough for neurological functions without significantly adding to the toxic load. Current protocols often prioritize lysine restriction more heavily.
- Role of Specialized Medical Formulas: Products like Glutarex 1 or specific XLys/XTrp formulations are indispensable. They provide a balanced mix of other essential amino acids, vitamins, minerals, and calories, ensuring normal growth and development while minimizing intake of problematic amino acids. These are prescribed and monitored by metabolic specialists.
- Overall Protein Moderation: In addition to specific amino acid restriction, overall dietary protein from whole foods is often carefully managed. For infants, breastfeeding might be supported due to its lower protein content compared to standard formulas. For older children, planned vegetarian or lower-protein diets can help reduce lysine and tryptophan intake. Carnitine supplementation, detailed later, supports these dietary efforts.
Essential Supplementation for Metabolic Support and Prevention
Beyond specialized diets, certain supplements are vital for supporting metabolic pathways and defending against GA1 complications. These work with dietary strategies to manage biochemical imbalances, minimize toxic buildup, and support overall health.
Key supplements include:
- L-Carnitine: This supplement plays an absolutely critical detoxification role. Carnitine binds to accumulating glutaric acid, forming glutarylcarnitine, which is then more easily excreted in urine. This lowers toxic metabolite levels and helps replenish the body's carnitine stores, often depleted by the ongoing detoxification effort (secondary carnitine deficiency). Consistent carnitine supplementation is fundamental for preventing severe neurological damage and supporting energy metabolism.
- Riboflavin (Vitamin B2): Riboflavin is considered because the GCDH enzyme requires a riboflavin derivative (FAD) to function. While it can't fix the genetic defect, ample riboflavin might maximize any residual GCDH enzyme activity in some individuals. It also supports other mitochondrial enzymes involved in energy production, contributing to overall metabolic efficiency.
- Ascorbic Acid (Vitamin C): This vitamin offers supportive benefits, especially during metabolic stress like illness. Vitamin C is a cofactor in collagen synthesis, a protein rich in lysine. By supporting collagen stability, it can help minimize the breakdown of body proteins during catabolic states, thus reducing the release of lysine that would otherwise be converted to glutaric acid. Its antioxidant properties also protect cells during stress.
Managing Acute Illness and Broader Preventive Considerations
Constant vigilance, especially during illnesses, is essential for individuals with GA1, as these periods carry a high risk of severe metabolic decompensation. Swift, proactive management of common ailments is crucial to prevent acute encephalopathic crises and further neurological injury.
Key strategies for acute illness and broader preventive care include:
- Prompt Management of Intercurrent Illnesses: Common illnesses can trigger catabolism (body protein breakdown), releasing lysine and tryptophan and rapidly increasing toxic metabolites. A vital "emergency" or "sick day" protocol involves immediate high-calorie (often glucose-based) intake, aggressive fever control, prompt infection treatment, and close contact with the metabolic team. Intravenous fluids may be needed if oral intake is insufficient.
- Avoiding Unnecessary Catabolic States: Any situation leading to catabolism, like prolonged fasting or poor appetite, must be managed to prevent toxic metabolite buildup. Consistent calorie intake, especially carbohydrates, through regular feeding, is crucial to provide energy and prevent protein breakdown, particularly during increased metabolic demand.
- Continuous Medical Oversight: Lifelong GA1 management requires a specialized metabolic team (physicians, dietitians, neurologists). Regular clinic visits for exams, developmental checks, and biochemical monitoring (blood, urine) are essential to adjust diet and supplements. Periodic neuroimaging may monitor brain health.
- Empowering Families Through Education: Thorough family education is fundamental. This includes understanding dietary needs, supplement importance, recognizing early crisis warning signs (irritability, lethargy, vomiting, new movement issues), and proficiency in emergency protocols—knowing when to increase calories, contact the metabolic team, and seek immediate medical help.