How to Treat Granular Corneal Dystrophy
What is Granular Corneal Dystrophy?
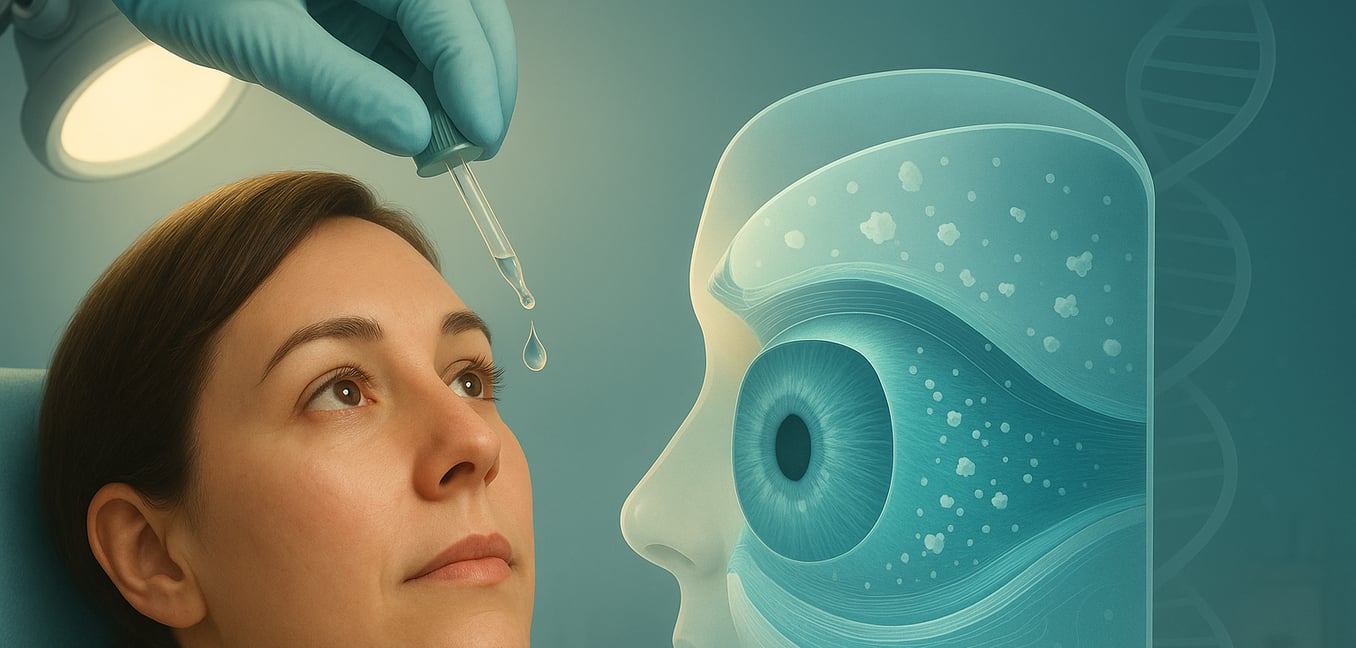
Granular Corneal Dystrophy (GCD) is a genetic eye condition that affects the cornea, the clear front surface of the eye. It is caused by a mutation in the TGFBI gene, which leads to the buildup of tiny, abnormal protein deposits in the cornea's middle layer, known as the stroma. Over time, these deposits, which can look like small breadcrumbs or snowflakes, make the cornea cloudy.
This cloudiness scatters light, causing symptoms like glare, light sensitivity, and eventually, a gradual decline in vision. In some cases, it can also lead to painful recurrent corneal erosions, where the cornea's surface layer breaks down and causes sharp pain, especially upon waking. While the condition progresses slowly, often over decades, various treatments are available to manage symptoms and restore sight.
Conservative and Non-Surgical Management
In the early stages of GCD, treatment focuses on managing symptoms to maintain comfort and quality of life. The following non-surgical strategies are commonly used to provide relief and improve visual clarity.
- Lubricating Eye Drops: Artificial tears and ointments keep the cornea moist, reducing friction from the eyelids and helping to prevent painful erosions. Special hypertonic saline drops can be prescribed to draw excess fluid from the cornea, reducing swelling and morning blurriness.
- Bandage Contact Lenses: If erosions become frequent or severe, an ophthalmologist may place a thin, protective soft lens on the eye. This lens acts as a shield over sensitive nerve endings, which dramatically reduces pain and creates a stable environment for the cornea to heal.
- Corrective Lenses: Updated prescriptions for glasses can help sharpen focus as vision changes. Lenses with anti-glare coatings or specific tints can minimize the disruptive glare and light sensitivity common with GCD. For some, rigid gas permeable (RGP) contact lenses may provide clearer vision than glasses by creating a smooth new surface over the irregular cornea.
Laser-Based Procedures for Vision Improvement
When glasses and contact lenses no longer provide adequate vision, or when recurrent erosions become unmanageable, an ophthalmologist may recommend a laser-based procedure. These techniques are designed to remove the corneal deposits that scatter light and impair vision. The most common of these is a procedure known as phototherapeutic keratectomy, or PTK.
PTK is a highly effective procedure that uses a cool ultraviolet beam from an excimer laser to precisely vaporize the superficial granular deposits. The goal is therapeutic: to smooth the corneal surface and clear the central visual axis of opacities. By ablating these deposits, the procedure significantly reduces the light scatter that causes debilitating glare and haze. This not only improves visual acuity but can also treat recurrent corneal erosions by creating a fresh surface for new cells to adhere to more strongly.
PTK is a quick outpatient procedure, typically taking only a few minutes. Afterward, a bandage contact lens is placed on the eye to protect the healing surface and minimize discomfort. Post-operative care is crucial and involves a strict regimen of antibiotic and anti-inflammatory eye drops to prevent infection and control healing. Vision will likely be blurry at first and will gradually improve over several weeks as the new, clear layer of surface cells regrows. It is important to understand that PTK is a treatment, not a cure. Because GCD is a progressive genetic condition, the deposits will eventually recur, though the benefits of PTK can last for many years before another treatment may be needed.
Corneal Transplants (Keratoplasty) for Severe Cases
When vision loss significantly impacts daily life or when deposits are too deep in the cornea for laser treatment, a corneal transplant (keratoplasty) may be recommended. This surgical approach involves replacing the diseased corneal tissue with healthy tissue from a donor.
Penetrating Keratoplasty (PKP)
PKP is a full-thickness transplant and has long been the standard for advanced corneal disease. In this procedure, the surgeon removes the central portion of the patient’s cloudy cornea and replaces it with a precisely matched, full-thickness button of donor tissue. The new cornea is sutured into place. While highly successful at restoring vision, this method has a longer recovery period and carries a higher risk of graft rejection, as it replaces all layers of the cornea.
Deep Anterior Lamellar Keratoplasty (DALK)
DALK is an advanced, partial-thickness transplant that is often the preferred technique for stromal dystrophies like GCD, where the innermost cell layer (the endothelium) is healthy. The surgeon carefully removes only the diseased outer layers—the epithelium and stroma—while preserving the patient’s own healthy endothelium. Retaining this layer dramatically lowers the long-term risk of graft rejection and results in a structurally stronger eye.
Post-Operative Care and Recurrence
Following any type of corneal transplant, strict adherence to a long-term regimen of steroid eye drops is essential to prevent the body’s immune system from rejecting the donor graft. Patients should also be aware that because GCD is a genetic condition, it can eventually recur in the new graft. The patient's own cells at the edge of the cornea can migrate onto the clear donor tissue and begin producing the abnormal protein deposits again, typically over 5 to 10 years.
Genetic Counseling and Future Directions
Because Granular Corneal Dystrophy is a hereditary condition, management can extend beyond treating an individual’s symptoms. Genetic counseling provides patients and their families with invaluable information about the autosomal dominant inheritance pattern of GCD, which means a child of an affected parent has a 50% chance of inheriting the gene mutation. This knowledge empowers families to make informed decisions and allows at-risk relatives to be monitored for early signs of the disease.
Looking ahead, researchers are exploring gene therapy as a way to stop the disease process at its source. One promising strategy is gene silencing, which uses tiny molecules called siRNA to intercept and neutralize the faulty instructions from the mutated TGFBI gene. This would prevent the abnormal protein from ever being produced, while allowing the healthy copy of the gene to function normally. An even more advanced approach is gene editing, using tools like CRISPR-Cas9. This technology acts like molecular scissors to find and permanently correct the mutation in the patient's own corneal cells. While still in early development, these therapies hold the potential to one day offer a permanent cure.