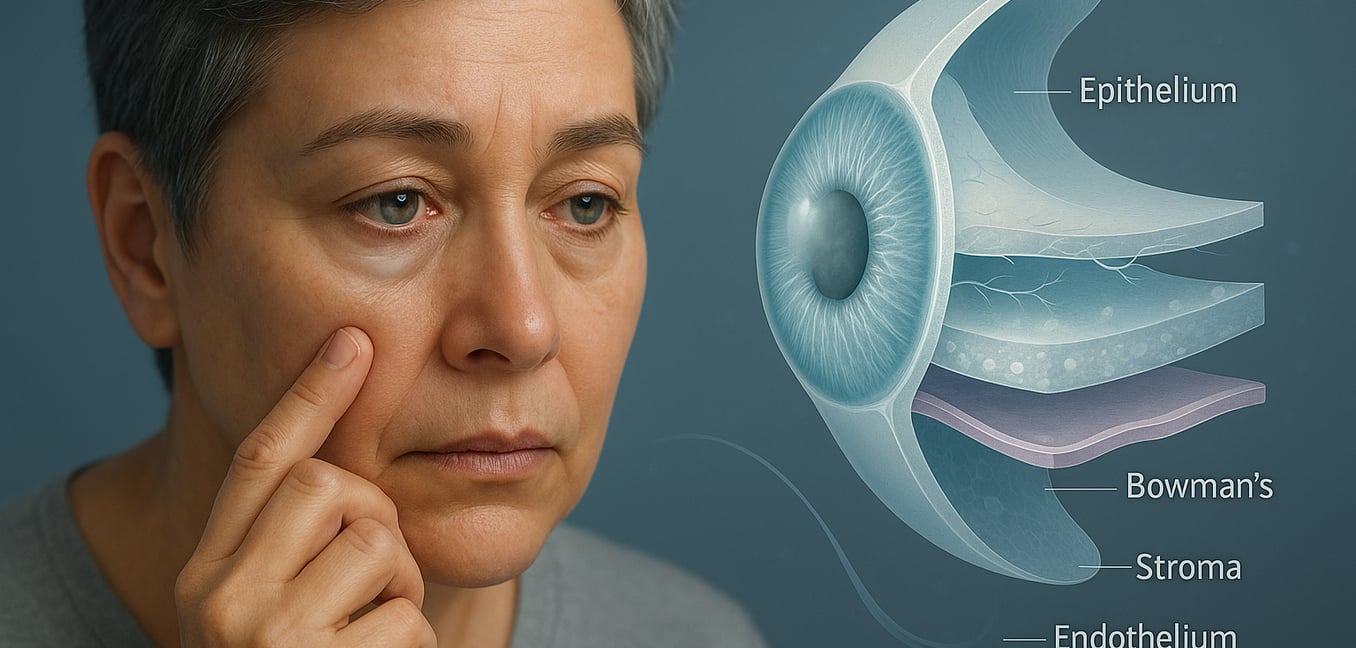
Corneal dystrophy is a group of inherited eye conditions characterized by the abnormal buildup of material in the cornea—the clear, front surface of the eye. This genetic disorder is progressive, meaning it slowly worsens over time and typically affects both eyes. As the material accumulates in one or more of the cornea's five layers, it can cause the cornea to become cloudy, swollen, or distorted.
Unlike eye problems caused by injury or infection, dystrophies are programmed by genetics. This slow deterioration of corneal clarity disrupts the eye's ability to focus light, leading to a range of complications that can severely impact vision and quality of life if left untreated. While gradual vision loss is a primary concern, some dystrophies introduce more immediate and painful complications.
Complication 1: Progressive and Disruptive Vision Loss
The most fundamental complication of untreated corneal dystrophy is a steady decline in the quality of vision. This is not a simple refractive error that can be fixed with stronger glasses; it is a structural problem within the eye's primary focusing surface. As abnormal material builds up or the cornea swells, it scatters light rather than focusing it cleanly onto the retina, leading to several disruptive symptoms.
- Blurring and Haze: Vision often becomes progressively foggy or hazy. For those with endothelial dystrophies like Fuchs', this blurriness can be most pronounced upon waking, as fluid accumulates in the cornea overnight.
- Glare and Halos: Corneal irregularities cause light from sources like headlights or street lamps to appear scattered, creating distracting starbursts or halos that make night driving hazardous.
- Light Sensitivity: Many people develop photophobia, where bright sunlight or even indoor lighting becomes uncomfortable or painful, forcing them to squint or wear dark glasses.
- Loss of Contrast and Color: As the cornea loses its transparency, it acts like a dirty lens, muting colors and reducing contrast. This can make it difficult to distinguish objects from their background, such as seeing a curb on a shaded street.
Complication 2: Chronic Pain from Recurrent Corneal Erosions
Beyond degrading vision, certain dystrophies that affect the cornea's outer layer can cause significant physical pain. These conditions weaken the bonds that anchor the surface epithelium to the underlying tissue, leading to a debilitating problem known as recurrent corneal erosions.
An erosion occurs when this fragile surface layer tears away, exposing the dense network of sensitive nerve endings beneath. This typically happens upon waking; during sleep, the eyelid can stick to the unstable corneal surface, and the simple act of opening the eyes in the morning is enough to rip the cells off. The result is a sudden, sharp pain, often described as feeling like sand or glass is in the eye. This initial pain triggers a cascade of other symptoms, including excessive watering, extreme light sensitivity, and blurred vision that can last for hours or days.
Complication 3: Infection, Ulcers, and Permanent Scarring
An intact cornea is a formidable barrier against pathogens. However, each time a recurrent erosion occurs, it creates an open wound on the eye's surface, leaving it vulnerable to infection from bacteria, viruses, or fungi. This significantly increases the risk of developing infectious keratitis, commonly known as a corneal ulcer.
A corneal ulcer is a medical emergency that can cause intense pain, discharge, and a rapid decline in vision. If not treated immediately and aggressively with antibiotics, it can lead to devastating consequences, including a perforation of the cornea or the formation of a dense, opaque scar that permanently blocks vision. In dystrophies affecting the inner endothelial layer, chronic swelling can also lead to painful blisters on the surface (bullous keratopathy), which can rupture and create a similar risk of infection and ulceration. Over time, repeated cycles of injury and healing can lead to permanent corneal scarring and the growth of new blood vessels into the normally clear cornea (neovascularization), causing irreversible vision loss.
End-Stage Disease: The Need for Surgical Correction
When the complications of corneal dystrophy—such as severe vision loss, chronic pain, or persistent swelling—become unmanageable with medical treatments like specialized eye drops, surgery becomes the most effective option. The goal of surgery is to replace the diseased corneal tissue with a healthy donor graft, thereby restoring the cornea's clarity and structural integrity.
For many years, the standard procedure was a full-thickness transplant (Penetrating Keratoplasty), which involved a long recovery period and a higher risk of complications. Today, surgical techniques have advanced significantly. For many types of dystrophy, surgeons can now perform partial-thickness transplants, such as Descemet Membrane Endothelial Keratoplasty (DMEK). These minimally invasive procedures replace only the specific diseased layers of the cornea, leaving healthy tissue intact. This targeted approach results in much faster visual recovery, better visual outcomes, and a lower risk of graft rejection, offering patients a definitive solution to restore their sight and quality of life.