Identifying the Most Common Corneal Dystrophy
The cornea is the transparent, dome-shaped window at the very front of your eye. It acts as the eye’s primary lens, bending light to help you see the world in sharp focus. When this vital structure is not perfectly clear and smooth, your vision can become compromised. While injury or infection can damage the cornea, a specific group of inherited conditions known as corneal dystrophies can also cause these changes.
Corneal dystrophies are genetic conditions passed down through families, resulting from an abnormal buildup of material in one or more of the cornea's layers. They are defined by a few key characteristics:
- They are inherited, meaning they are caused by a variation in a person’s genes. If a patient is diagnosed, their close relatives may also have the condition, even without symptoms.
- They are almost always bilateral, affecting both eyes. However, the severity is often asymmetric, with one eye showing signs earlier or more significantly than the other.
- They are slowly progressive, developing gradually over many years or even decades. They are also non-inflammatory, meaning they are not associated with the redness or discharge seen in eye infections.
- They are not linked to systemic diseases. These are standalone eye conditions, not a complication of other health problems like diabetes or autoimmune disorders.
Epithelial Basement Membrane Dystrophy (EBMD)
Of the many types of corneal dystrophies, one is far more common than all the others: epithelial basement membrane dystrophy, or EBMD. Because a large number of people with EBMD have no symptoms, they may have the condition without ever realizing it.
What Is EBMD? The Root of the Problem
At its core, EBMD is a problem of poor adhesion in the cornea’s outermost layer, the epithelium. This layer of surface cells must anchor itself to a foundation called the basement membrane. In EBMD, this membrane is produced abnormally, acting less like strong glue and more like a weak adhesive. This faulty foundation causes the surface cells to be loose and unstable, creating an irregular surface that can disrupt the tear film and scatter light, leading to blurry vision. This instability is also why the top layer is more susceptible to tearing away, a painful complication known as recurrent corneal erosion (RCE).
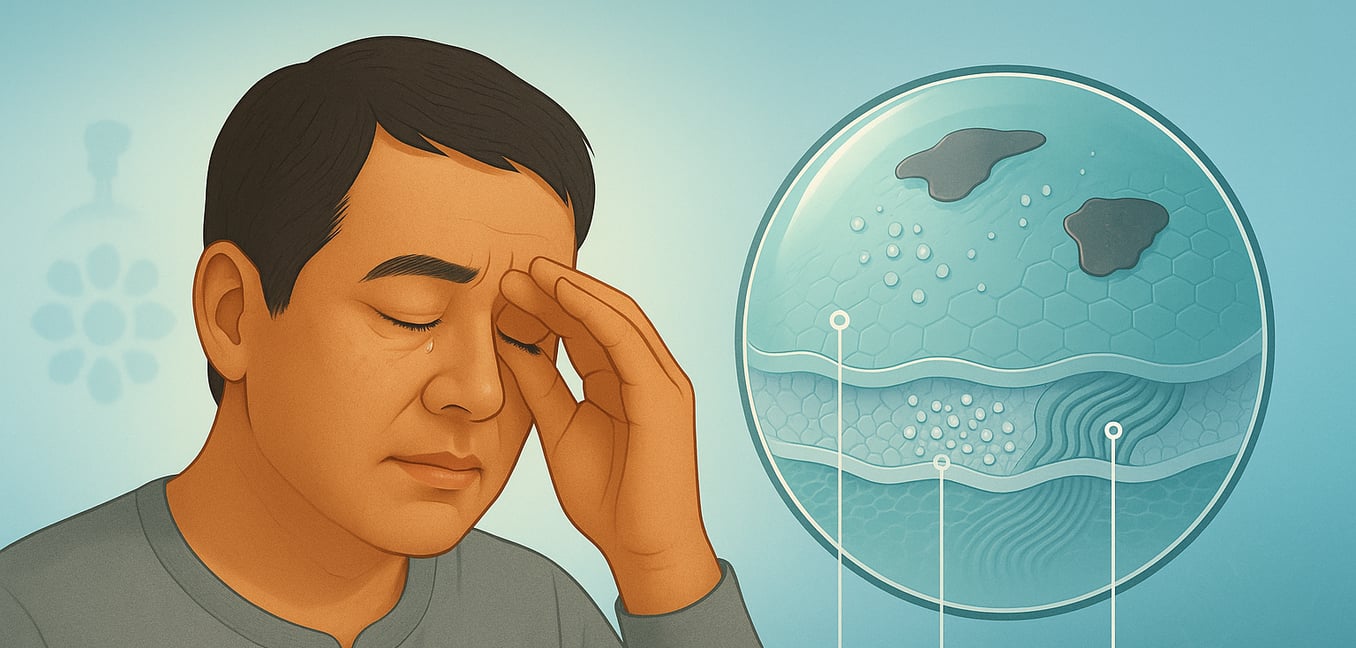
The "Map-Dot-Fingerprint" Signs
EBMD is often called map-dot-fingerprint dystrophy, a descriptive nickname that accurately portrays what an eye doctor sees during a slit-lamp examination. Each part of the name corresponds to a distinct clinical sign:
- Map Patterns: These are large, grayish, and irregularly shaped patches on the corneal surface. With distinct borders that can resemble coastlines on a globe, these patterns are created by thickened, redundant layers of the basement membrane pushing up into the surface epithelium.
- Dot Opacities: These are small, gray-white opacities that are actually tiny cysts filled with trapped cellular debris. They form because the disorganized surface cells cannot mature and shed in a normal, orderly fashion.
- Fingerprint Lines: These are fine, parallel, and often swirling ridges that resemble the whorls of a human fingerprint. They are formed by thin folds or duplications within the abnormal basement membrane material itself.
Symptoms and Complications
While many individuals with EBMD are completely asymptomatic, others experience mild but persistent issues. The most common complaints are a gritty, foreign body sensation and vision that is blurry or fluctuates throughout the day. This visual disturbance is not caused by a need for new glasses but by an unstable tear film and irregular astigmatism from the uneven corneal surface.
The most significant complication is recurrent corneal erosion (RCE), which affects about 10% of people with EBMD. This occurs when the poorly attached surface layer tears away, often upon waking up. It causes sudden, sharp pain, intense light sensitivity, and excessive tearing.
Why Diagnosis Matters for Eye Surgery
Identifying EBMD is critical before a patient undergoes any type of refractive surgery (like LASIK) or cataract surgery. The irregular surface it creates can interfere with the highly precise measurements needed to calculate the power of an intraocular lens or to plan a laser treatment. Failing to diagnose and manage EBMD beforehand can lead to inaccurate calculations and suboptimal vision after surgery.
How EBMD Is Managed
Managing EBMD is tailored to the severity of the symptoms, ranging from simple eye drops to minor surgical procedures. The goal is to improve comfort, stabilize vision, and prevent painful erosions.
Managing Daily Symptoms
For those with mild, chronic symptoms, treatment focuses on improving the health of the eye's surface. This often starts with hypertonic saline drops or ointments, which help draw excess fluid from the cornea and encourage better cell adhesion, especially when used overnight. Aggressively treating any co-existing conditions like dry eye or blepharitis (eyelid inflammation) is also key. This may involve therapies like medicated eye drops, lid hygiene, or punctal plugs to preserve tears on the eye’s surface.
Treating Painful Recurrent Erosions
When a recurrent corneal erosion occurs, treatment becomes more intensive to heal the immediate abrasion and prevent it from happening again. A soft bandage contact lens is often placed on the eye for several days or weeks to protect the delicate, healing surface from the friction of the eyelid. To calm surface inflammation that can hinder healing, an eye doctor may prescribe a short course of topical steroids and an oral antibiotic like doxycycline.
Advanced and Surgical Interventions
For persistent cases of RCE that do not respond to other treatments, more advanced options may be necessary. These can range from biologic eye drops and amniotic membranes that promote healing to surgical procedures. Common interventions include:
- Anterior Stromal Puncture: A procedure where a fine needle is used to create tiny punctures through the basement membrane. This induces a small scarring response that helps "spot weld" the epithelial layer to the underlying cornea.
- Diamond Burr Polishing: A technique where a specialized, fine-bristled burr is used to gently polish away the abnormal basement membrane, creating a smoother, healthier foundation for new cells to adhere to.
- Phototherapeutic Keratectomy (PTK): A laser-based procedure that precisely removes the compromised surface layers, allowing for the regrowth of a more stable and regular epithelium.