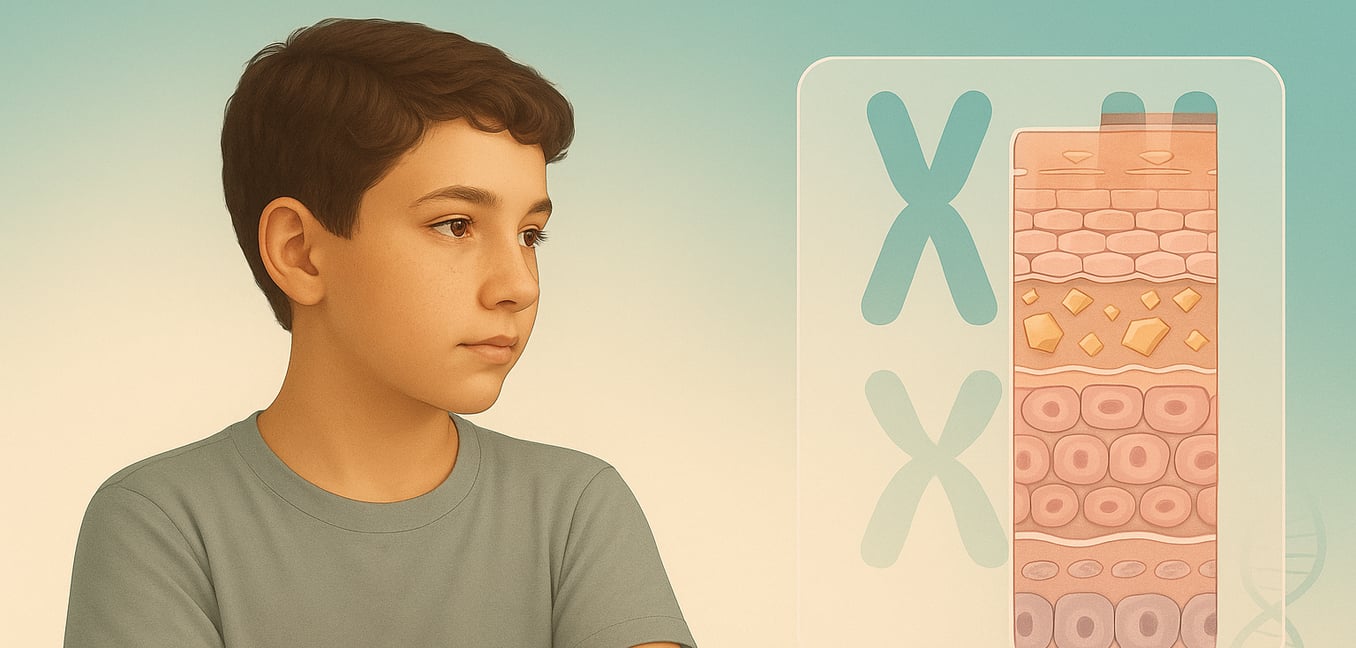
What is Recessive X-Linked Ichthyosis?
Recessive X-linked ichthyosis (XLRI) is the second most common inherited form of ichthyosis, a group of genetic skin disorders characterized by dry, scaly skin. Due to its X-linked inheritance pattern, it almost exclusively affects males, with an incidence of about 1 in every 2,500 to 6,000 boys. The condition is caused by a mutation or deletion in the STS gene, which is located on the X chromosome.
This genetic fault prevents the body from making a vital enzyme called steroid sulfatase. In the skin, this enzyme's job is to help break down a substance called cholesterol sulfate. Without the enzyme, cholesterol sulfate builds up in the outermost layer of the skin. This buildup acts like a strong glue, preventing dead skin cells from shedding in a normal, orderly process. This impaired shedding, known as desquamation, causes skin cells to stick together, resulting in the thick, scaly skin (hyperkeratosis) that defines the condition. This single enzyme deficiency leads to a wide range of symptoms, affecting not only the skin but other body systems as well.
Primary Symptoms: The Skin
The skin manifestations are the most visible and defining feature of XLRI. The hallmark of the condition is the presence of scales that are typically large, polygonal (many-sided), or rhombic (diamond-shaped). These scales are often dark brown or grayish and are tightly stuck to the skin's surface. This can create a "dirty" or unwashed appearance, particularly around the neck, behind the ears, and on the trunk. While this classic look is common, some individuals may have much finer, lighter scales that can be mistaken for the more common ichthyosis vulgaris, sometimes delaying a correct diagnosis.
The scaling follows a distinct and symmetrical distribution pattern that is a key diagnostic clue. It is most prominent on the extensor surfaces of the limbs (such as the shins and the backs of the forearms), the torso, and the scalp, where it can cause significant flaking. Crucially, certain areas are characteristically spared, including the palms of the hands, the soles of the feet, and the major body folds, like the creases of the elbows and the backs of the knees. The hair and nails are typically unaffected.
The severity of the skin symptoms is not static and often fluctuates with the environment. Many people with XLRI find their skin improves dramatically during warm, humid summer months, especially with sun exposure. Conversely, the condition tends to worsen significantly during the cold, dry winter months, leading to increased dryness, scaling, and discomfort.
Associated Symptoms: Beyond the Skin
Because the steroid sulfatase enzyme is active in tissues throughout the body, its absence makes XLRI a multi-system disorder. A number of important non-skin symptoms can develop, which are crucial for comprehensive diagnosis and management.
Ocular and Testicular Findings
About half of all adult males with XLRI develop small, dot-like deposits deep within the cornea, the clear front surface of the eye. These opacities are asymptomatic, meaning they do not affect vision, and are usually only detected during a specialized eye exam. They can also be found in about 25% of female carriers, serving as a subtle clue to their genetic status.
One of the most common associated conditions is cryptorchidism, where one or both testicles fail to descend into the scrotum before birth. This affects approximately 5-20% of boys with XLRI, a rate far higher than in the general population. Its presence is a significant red flag for pediatricians and often requires urological monitoring or intervention to prevent long-term complications, such as impaired fertility and an increased risk of testicular cancer.
Neurological and Cognitive Impact
The steroid sulfatase enzyme is also active in the brain, where it influences neurosteroid levels. Consequently, its deficiency is directly linked to a higher prevalence of certain neurodevelopmental conditions. Studies show that attention-deficit hyperactivity disorder (ADHD) may affect up to 40% of individuals with XLRI, and autism spectrum disorder is also more common. These are considered core features of the disorder itself, not just a psychological response to living with a chronic skin condition. Female carriers also show an increased risk for these and other behavioral traits.
Contiguous Gene Syndromes
In about 10% of cases, XLRI is caused by a large genetic deletion that removes the STS gene along with several neighboring genes. This results in more complex "contiguous gene syndromes." For example, if the deletion includes a nearby gene, it can cause Kallmann syndrome, which combines ichthyosis with impaired sexual development and a loss of the sense of smell (anosmia). Larger deletions can lead to other features, such as intellectual disabilities or short stature.
Other Systemic Conditions
Research has uncovered links to other health issues. For instance, men with XLRI, particularly between the ages of 40 and 69, have a higher incidence of atrial fibrillation or flutter, a type of irregular heartbeat. Additionally, the thickened skin can physically block sweat glands, leading to a reduced ability to sweat (hypohidrosis) in nearly 20% of patients. This impairs the body's ability to cool down, increasing the risk of overheating and heat intolerance during exercise or in hot weather.
Onset and Progression Over a Lifetime
The timeline of XLRI is unique, as the first clues can appear even before birth. The symptoms then emerge in early infancy and evolve, persisting as a lifelong condition.
The earliest signs may manifest during the final stages of pregnancy. Because the steroid sulfatase enzyme is also produced by the placenta, its deficiency can impair the production of hormones needed to initiate childbirth. As a result, mothers carrying an affected male fetus often experience prolonged or difficult labor, which may require medical intervention like a Cesarean section. This obstetric history is a notable retrospective sign of the condition.
While some infants are born with temporary, mild redness and peeling, it is more common for the skin to appear normal at birth. The characteristic scaling typically develops within the first few weeks to months of life. It may begin as fine, generalized flaking before progressing into the larger, darker, and more adherent scales that become prominent throughout childhood. The ichthyosis itself is a persistent condition, though its severity can fluctuate with the seasons. As individuals with XLRI age, other features may become apparent. The dot-like corneal deposits, for example, are rarely seen in children but are found in about 50% of affected adult males, representing a late-onset feature of the disorder.