A Guide to Treating Congenital Toxoplasmosis
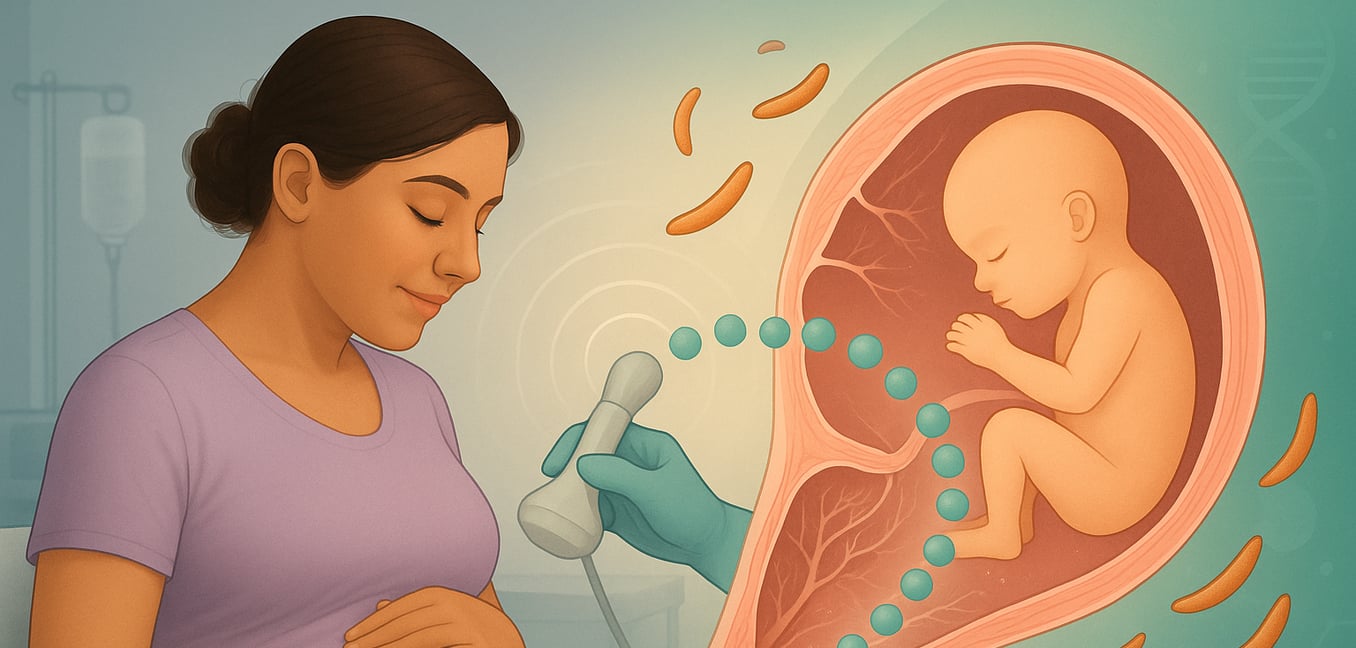
Congenital toxoplasmosis is an infection that occurs when the Toxoplasma gondii parasite is passed from a mother to her unborn baby during pregnancy. While the mother may experience few symptoms, the infection can cause serious health problems for the infant. Effective medical intervention, both before and after birth, is critical to manage the infection and reduce the risk of long-term complications.
Preventing Transmission During Pregnancy
When a pregnant woman is diagnosed with a new toxoplasmosis infection, the primary goal is to prevent the parasite from reaching the fetus. This involves a proactive treatment approach designed to act as a protective barrier.
- Initial Treatment with Spiramycin: Following a maternal diagnosis, doctors typically prescribe spiramycin. This antibiotic concentrates in the placenta, creating a shield that helps reduce the chance of the parasite crossing over to the developing baby. It is generally considered safe during pregnancy and is used as a first line of defense.
- Confirming Fetal Infection: An amniocentesis may be recommended, usually after 18 weeks of gestation, to test the amniotic fluid for the parasite's DNA. This test determines if the fetus has already been infected, which is crucial for guiding the next steps in treatment.
- Escalating Therapy: If the amniocentesis confirms the fetus is infected, the treatment strategy changes. The care team will switch from spiramycin to a more potent combination of pyrimethamine and sulfadiazine. This regimen can cross the placenta to directly treat the infection in the fetus, helping to lessen its severity before birth.
- The Importance of Timing: The risk of transmission and the potential severity of the infection depend on when the mother was infected. An infection early in pregnancy has a lower transmission risk but can cause more severe harm if it occurs. An infection later in pregnancy is more likely to be transmitted, but the resulting illness in the infant is often less severe.
The Standard Treatment for Infected Infants
For infants born with congenital toxoplasmosis, the "gold standard" of care is a combination therapy designed to attack the parasite from multiple angles. Treatment is intensive and typically lasts for one year to manage active symptoms and prevent future complications.
- Pyrimethamine: This is the primary anti-parasitic drug. It works by blocking an enzyme the parasite needs to use folic acid, which stops it from replicating. Because it can also affect the patient's bone marrow, regular blood tests are required to monitor for side effects like anemia.
- Sulfadiazine: This antibiotic works with pyrimethamine to create a powerful "one-two punch." It targets a different step in the same folic acid pathway, making it very difficult for the parasite to survive.
- Leucovorin (Folinic Acid): This is not an anti-parasitic drug but a vital "rescue" agent. It protects the infant's body from pyrimethamine's effects by providing a form of folic acid that human cells can use but the parasite cannot. This makes the long-term treatment safer and more tolerable.
Alternative Treatment Regimens
When the standard therapy is not suitable due to allergies or side effects, healthcare providers have several effective alternatives.
- Clindamycin: This antibiotic is often used with pyrimethamine as a substitute for sulfadiazine, especially in cases of a sulfa allergy. While effective against toxoplasmosis, it can cause gastrointestinal side effects and requires careful monitoring.
- Trimethoprim-sulfamethoxazole (TMP-SMX): This combination drug, available as a single pill, also disrupts the parasite's folic acid pathway. Some studies suggest it can be as effective as the standard regimen and may be better tolerated. It is also a valuable option when pyrimethamine is unavailable.
- Atovaquone: This medication works by targeting the parasite's energy production. It can be combined with other drugs or used alone if a patient is intolerant to multiple standard medications. However, its use in infants is less studied, and dosing can be complex.
- Azithromycin: In some cases, this antibiotic has been used in combination with pyrimethamine. However, there is limited data to support its routine use for treating active congenital toxoplasmosis in infants.
Supportive Care and Long-Term Management
Treating congenital toxoplasmosis is a long-term commitment that extends beyond anti-parasitic drugs. A comprehensive plan includes supportive therapies and diligent monitoring to manage both the infection and the side effects of treatment.
Using Corticosteroids for Inflammation
In cases of severe inflammation of the brain or eyes, corticosteroids like prednisone may be added to the treatment plan. They are used for the shortest possible time to reduce swelling and prevent organ damage. Because steroids suppress the immune system, they are administered cautiously only when necessary.
Managing Seizures
Anticonvulsant medications are prescribed only if a child develops seizures as a result of the infection. These drugs help control neurological symptoms during the acute phase of treatment and are not given preventatively.
Essential Monitoring
Ongoing monitoring is a cornerstone of safe treatment. This includes regular blood tests to watch for bone marrow suppression from pyrimethamine, allowing the medical team to adjust the leucovorin dose as needed. The team also stays vigilant for reactions to other drugs, such as rashes or kidney issues from sulfadiazine, ensuring side effects are managed promptly.