What is the Best Treatment for Keratoconus?
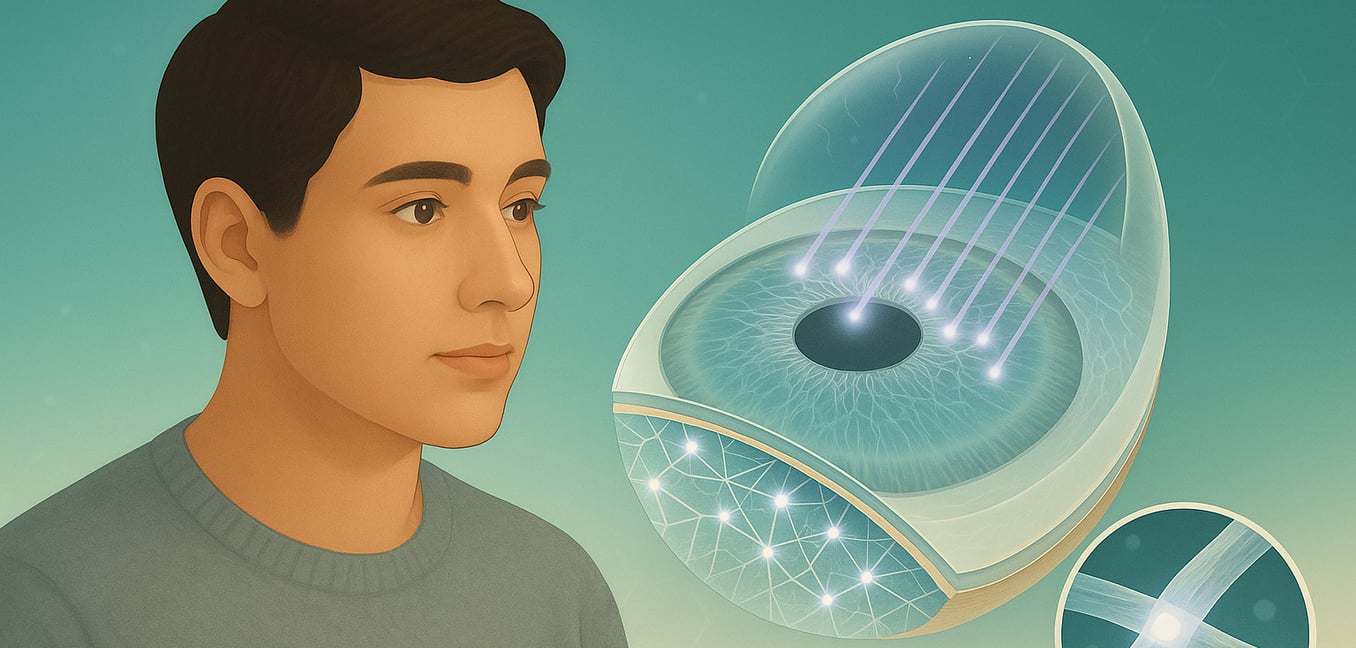
Keratoconus is a progressive eye disorder where the cornea—the clear, dome-shaped front surface of the eye—thins and bulges outward into a cone shape. This structural change is caused by the weakening of the cornea's natural collagen fibers. As the cornea becomes irregular, it can no longer focus light correctly, leading to distorted, blurry vision and increased sensitivity to light and glare. While the exact cause is unknown, genetics and chronic eye rubbing are major risk factors. The condition typically appears in the late teens and can worsen into a person's 30s, making early diagnosis and treatment essential to preserve vision.
The "best" treatment for keratoconus isn't a single procedure but rather a personalized plan that depends on your specific goals. Treatment is divided into two main categories: first, halting the progression of the disease, and second, improving the vision that has already been affected.
Step 1: Halting Progression with Corneal Cross-Linking
For anyone with active, progressing keratoconus, the primary goal is to stop the disease from getting worse. The only proven treatment to achieve this is corneal collagen cross-linking (CXL), a minimally invasive therapy designed to strengthen the cornea and prevent further bulging.
Epithelium-Off (Epi-Off) CXL
This is the original and most established method. A surgeon first gently removes the cornea's thin outer layer, the epithelium. This allows special riboflavin (vitamin B2) eye drops to fully penetrate the corneal tissue. The eye is then exposed to a controlled ultraviolet-A (UVA) light, which activates the riboflavin and creates strong new bonds between collagen fibers, making the cornea more rigid.
Epithelium-On (Epi-On) CXL
Developed to increase comfort and reduce recovery time, this technique leaves the protective epithelial layer intact. Because the epithelium acts as a natural barrier, this approach requires special riboflavin formulations or techniques to help the drops absorb. While it offers a more comfortable experience, its effectiveness at halting progression may not be as robust as the epi-off method in all cases.
Accelerated Cross-Linking
This newer protocol significantly shortens the treatment time. Instead of the standard 30-minute UVA exposure, accelerated CXL uses a higher-intensity light for a much shorter duration, often just a few minutes. Studies have shown this faster protocol can be just as effective at stabilizing the cornea, offering greater convenience for the patient.
Once cross-linking has successfully stabilized the cornea, the focus shifts from preventing further damage to improving the vision that has already been affected.
Step 2: Improving Vision After Stabilization
After progression is halted, the next step is to correct the distorted vision caused by the cone-shaped cornea. This is typically managed with a tiered approach, starting with the least invasive options.
Glasses and Standard Contact Lenses
In the very early stages of keratoconus, prescription glasses or standard soft contact lenses may be sufficient to provide clear vision. However, as the cornea becomes more irregular, these options lose their effectiveness.
Rigid Gas Permeable (RGP) Lenses
Often the first line of defense for moderate keratoconus, these "hard" lenses provide a smooth, uniform surface over the irregular cornea. An RGP lens holds its own shape, creating a new, clear focusing surface for the eye. The space between the lens and the cornea fills with tears, which helps neutralize the irregularities and deliver crisp vision.
Hybrid and Piggyback Lenses
For those who find RGP lenses uncomfortable, hybrid lenses offer a "best of both worlds" solution. They feature a hard RGP center for sharp vision fused to a soft outer skirt for comfort. A similar approach is the "piggyback" system, where a standard RGP lens is worn on top of a soft contact lens, which acts as a comfortable cushion.
Scleral Lenses
These large-diameter lenses are a game-changer for moderate to advanced keratoconus. Scleral lenses completely vault over the irregular cornea without touching it, resting instead on the less sensitive white part of the eye (the sclera). This creates a fluid-filled reservoir between the lens and the cornea that masks surface irregularities, providing exceptionally clear, stable vision and all-day comfort.
Surgical Options for Vision Improvement
When contact lenses no longer provide adequate vision or become too difficult to wear, surgical intervention may be the next step. These procedures aim to physically reshape the cornea to improve its focusing power.
Intrastromal Corneal Ring Segments (ICRS)
This procedure is ideal for patients with mild to moderate keratoconus who cannot tolerate contact lenses but do not yet need a full transplant. A surgeon inserts one or two tiny, clear, semi-circular plastic rings into the cornea's middle layer. These rings flatten the central cone, making the corneal surface more regular. This not only improves vision with glasses but can also make it possible to wear contact lenses again comfortably. ICRS is often combined with CXL to lock the improved corneal shape in place.
The Future of Keratoconus Care
Research is constantly advancing toward less invasive and more restorative treatments. The future of keratoconus therapy is focused on triggering the body's own healing processes to repair the cornea.
Medicated Eye Drops for Cross-Linking
A promising therapy in development involves eye drops that could strengthen the cornea without any surgery or UV light. These drops aim to trigger the body's natural collagen cross-linking process, offering a potential future where treatment is as simple as a daily medication.
Regenerative Medicine
Scientists are exploring "cell-free" therapies using tiny particles secreted by stem cells. These particles are rich in healing signals that could prompt a patient's own corneal cells to repair damaged structures and rebuild a healthier tissue matrix, potentially reversing some of the damage caused by the disease.
Advanced Ring Segments from Donor Tissue
Building on the success of synthetic rings, a newer technique uses precisely shaped rings crafted from human donor corneal tissue. Because the implant is made of natural material, it may integrate more seamlessly into the patient's cornea, reducing the risk of complications while providing structural support.