Understanding Omphalocele: A Brief Overview
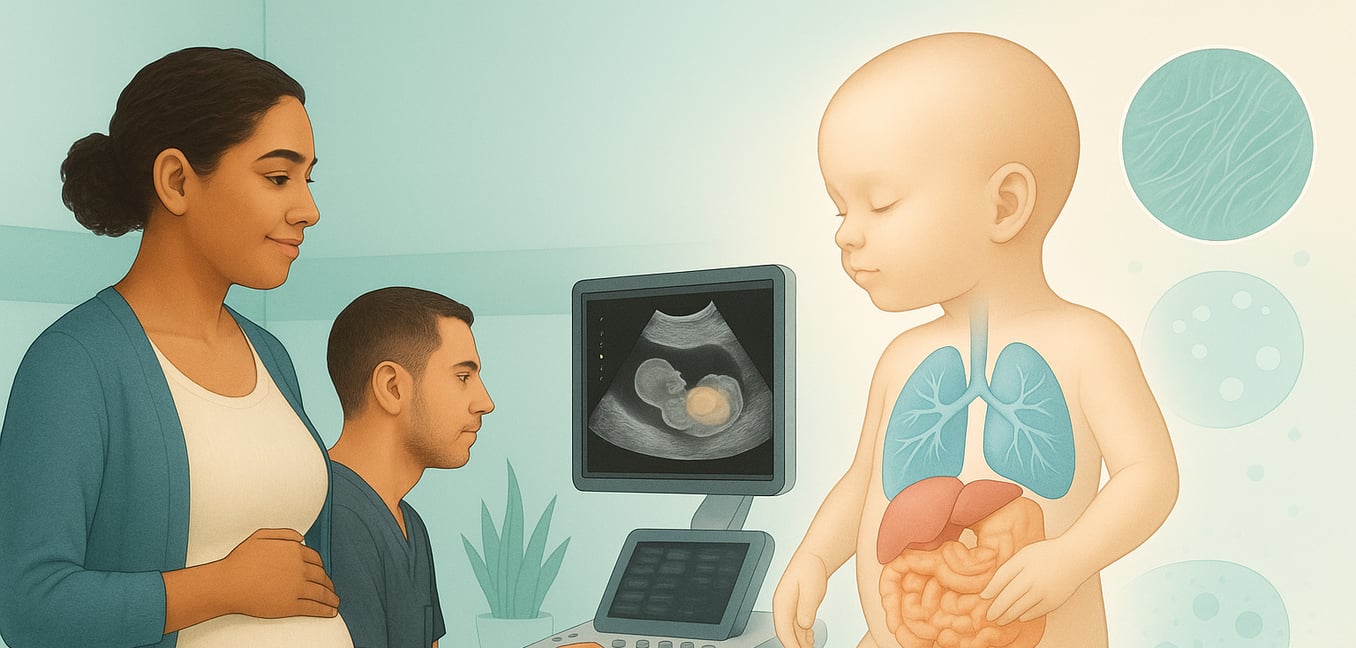
Omphalocele, also known as exomphalos, is a congenital abdominal wall defect where an infant's abdominal organs, such as the intestines and liver, protrude through the umbilical ring. These organs are enclosed in a protective, transparent sac, a key feature that distinguishes it from similar conditions like gastroschisis. The size of the defect can range from small to giant, a factor that significantly impacts management.
The prognosis for omphalocele is heavily influenced by the presence of associated conditions. A high percentage of cases are linked to chromosomal abnormalities, like trisomy 18 and 13, and structural malformations, especially of the heart. For this reason, an omphalocele diagnosis, typically made via routine ultrasound, prompts a comprehensive evaluation to determine if it is an isolated issue or part of a larger syndrome. This information is vital for counseling families and planning perinatal care.
First Line of Detection: The Crucial Role of Prenatal Ultrasound
The initial diagnosis of omphalocele is almost always made during a routine prenatal ultrasound. This non-invasive scan provides the first look at the developing fetus and can identify the characteristic protrusion of organs at the umbilical cord site, setting the stage for a complete evaluation. A detailed, high-resolution ultrasound provides much more than a simple diagnosis; it offers a comprehensive picture by focusing on several key areas:
- Confirm the diagnosis. While the defect can be seen in the first trimester, a definitive diagnosis is usually made after 12 weeks of gestation to distinguish it from the normal, temporary herniation of the midgut. Sonographers look for the tell-tale sign: a membrane-covered sac containing abdominal organs.
- Characterize the defect and its contents. Ultrasound is used to measure the defect's size and identify which organs are herniated, especially the liver. This information is critical for predicting surgical complexity and the potential risk of underdeveloped lungs.
- Survey for other abnormalities. Because omphalocele is often linked to other issues, the ultrasound includes a meticulous, head-to-toe examination. A fetal echocardiogram, a specialized ultrasound of the heart, is standard practice to screen for associated cardiac defects.
- Guide further testing. Based on the findings, the care team will recommend next steps. This almost always includes an offer of comprehensive genetic testing, such as amniocentesis. In complex cases, a fetal MRI may be recommended to gain more detailed information.
A Deeper Look: The Use of Fetal MRI for Enhanced Evaluation
While ultrasound is excellent for initial diagnosis, fetal magnetic resonance imaging (MRI) offers a deeper, more detailed view that is crucial for managing complex cases. This advanced imaging technique complements ultrasound by providing superior anatomical detail and more accurate measurements.
- Precisely measure lung volume. One of MRI's greatest strengths is its ability to assess lung development. It allows for an accurate calculation of the baby's lung size compared to the expected size for their gestational age. A low ratio is the most reliable sign of underdeveloped lungs (pulmonary hypoplasia), helping the team anticipate the baby's breathing needs after birth.
- Provide enhanced anatomical detail. MRI provides a clearer, more detailed view of the baby's organs. It can precisely map the amount of liver outside the abdomen and its blood supply, which is vital information for the surgical team. This detail also helps confirm the contents of the sac and assess the size of the abdominal cavity.
- Offer a comprehensive second look. MRI is not limited by factors like fetal position or maternal body size in the same way ultrasound can be. It is particularly effective at evaluating the fetal brain and spine for subtle abnormalities, ensuring the care team has the most complete diagnostic information possible for accurate counseling.
From Image to Action: How Prenatal Scans Shape Prognosis and Treatment
The detailed information gathered from prenatal imaging serves as a crucial roadmap, allowing the medical team to predict challenges, counsel the family, and develop a highly individualized care plan. This transforms prenatal scans from simple diagnostic tools into essential guides for postnatal management.
Planning for Delivery and Surgical Repair
Key findings like the size of the defect and liver involvement directly influence the surgical strategy. A small, isolated omphalocele may be suitable for a primary repair in a single operation shortly after birth. In contrast, a giant omphalocele containing the liver, as seen on ultrasound or MRI, signals the need for a staged repair over weeks or months to avoid a dangerous spike in abdominal pressure. This information also dictates delivery at a tertiary care center with immediate access to a neonatal intensive care unit (NICU) and pediatric surgeons. A planned cesarean section may be considered to protect a large, liver-filled sac from damage during labor.
Anticipating Respiratory Needs
The lung volume ratio calculated from a fetal MRI is a powerful predictor of respiratory health. A low ratio is a clear warning of pulmonary hypoplasia. This finding allows the team to prepare for immediate intubation and mechanical ventilation after birth and to counsel parents about a potentially longer NICU stay, an increased risk of pulmonary hypertension (high blood pressure in the lungs), and a more guarded respiratory outlook. The team can also have equipment ready to protect the omphalocele sac and place a nasogastric tube to decompress the stomach.
Determining Overall Prognosis
Ultimately, the presence or absence of other structural or chromosomal abnormalities is the most critical factor. When imaging confirms the omphalocele is an isolated defect—with a normal heart, brain, and kidneys—the prognosis is generally excellent with a high survival rate. However, if imaging reveals a severe co-occurring heart defect or other major malformations, the outlook becomes far more complex. These associated findings often have a greater impact on the infant’s survival and long-term health than the omphalocele itself, making a thorough imaging survey essential for accurate family counseling.