Macular corneal dystrophy is a rare, inherited condition that affects the cornea, the clear front part of the eye. It is classified as a stromal dystrophy, meaning it primarily impacts the stroma, which is the thickest middle layer of the cornea. Unlike some other corneal dystrophies, it is passed down in a recessive inheritance pattern, making it less common but often more severe. The condition causes dense, greyish-white deposits to accumulate within the stroma, gradually making it cloudy and impairing vision. These changes can also cause the cornea to become thinner and its surface irregular, leading to painful erosions and sensitivity to light. Because macular corneal dystrophy typically causes significant vision loss between the ages of 20 and 40, understanding the treatment options is crucial for managing the condition and preserving sight.
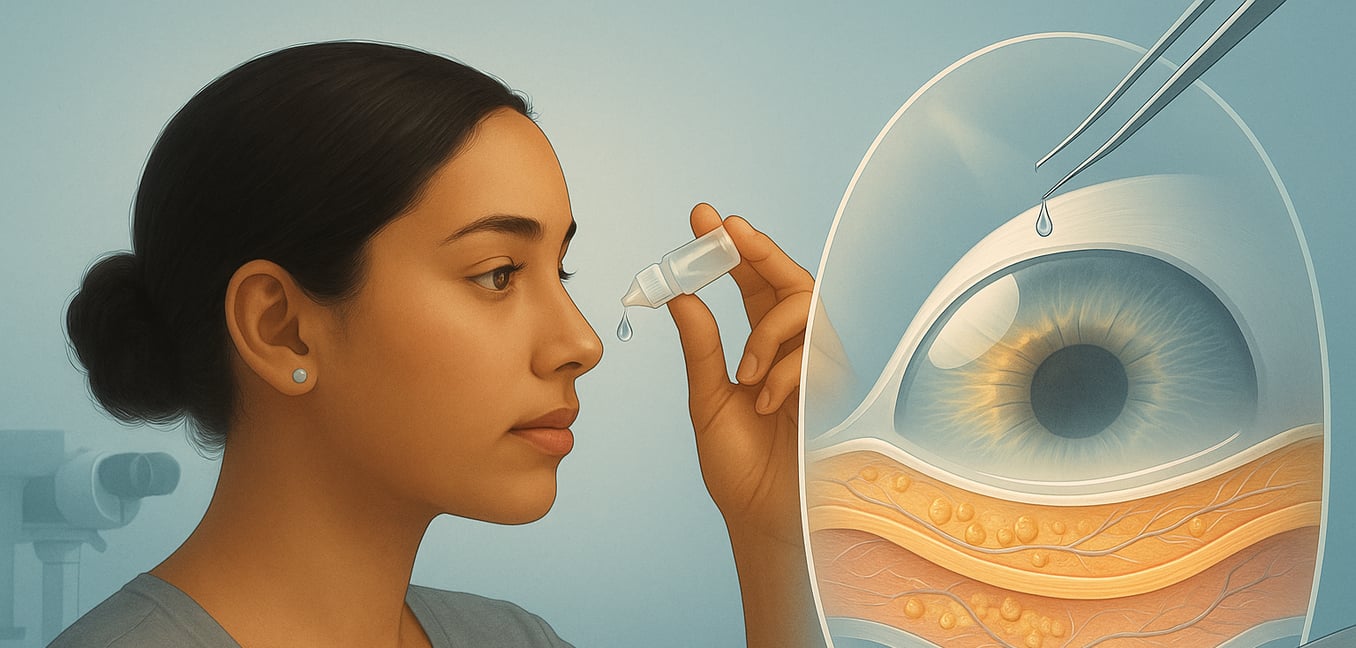
In the early stages of macular corneal dystrophy, or for managing specific symptoms, treatment focuses on providing comfort and protecting the eye's surface. As the disease progresses, the corneal surface can break down, causing painful recurrent erosions that feel like something is stuck in the eye. To manage this, an eye doctor may recommend lubricating eye drops, gels, or ointments to keep the cornea moist and prevent the eyelid from sticking to the fragile surface, which can reduce discomfort and aid healing. If the corneal surface is broken, antibiotic eye drops may be prescribed to prevent infection. In some cases, special "bandage" contact lenses can be worn to cover the cornea, protecting it from the friction of the eyelids and allowing erosions to heal. While these treatments can effectively manage pain and light sensitivity, they do not address the underlying cause of vision loss, which is the progressive clouding of the stroma.
When vision becomes significantly impaired, a corneal transplant, also known as keratoplasty, is the most effective treatment for restoring sight. This surgical procedure involves replacing the diseased cornea with a healthy one from a donor. For macular corneal dystrophy, surgeons typically perform one of two types of transplants:
- Penetrating Keratoplasty (PK): This is the traditional full-thickness corneal transplant, where the entire central part of the patient's cornea is removed and replaced with a donor cornea. PK has a long history of success in treating macular corneal dystrophy and effectively restores clarity to the visual axis.
- Deep Anterior Lamellar Keratoplasty (DALK): This is a more advanced partial-thickness transplant where only the diseased outer and middle layers of the cornea (the epithelium and stroma) are replaced, leaving the patient’s own healthy innermost layer (the endothelium) in place. DALK is often preferred because preserving the patient's endothelium can lead to a lower risk of graft rejection and better long-term graft survival. The choice between PK and DALK depends on the specific condition of the cornea and the surgeon's expertise. Although a transplant can successfully restore vision for many years, the dystrophy can eventually recur in the new donor tissue. However, this recurrence typically happens slowly over a long period.
How fast does corneal dystrophy progress?
The progression rate of corneal dystrophy varies significantly depending on the specific type of the disease. Many forms, such as Fuchs dystrophy and posterior polymorphous dystrophy, progress very slowly over several decades, with symptoms often appearing later in life. For instance, Fuchs dystrophy may develop over 10 to 30 years, and some people may remain asymptomatic for a long time. In contrast, other types like macular corneal dystrophy and gelatinous drop-like dystrophy can progress more rapidly, causing severe vision loss early in life that often requires surgical intervention. Ultimately, while some individuals experience only mild symptoms that change little over time, others may face a quicker decline in vision.
Can you drive with corneal dystrophy?
The ability to drive safely with corneal dystrophy depends on the specific type and severity of your condition, but for many, it can be challenging, particularly at night. For instance, patients with Fuchs’ dystrophy or Granular Corneal Dystrophy Type 2 (GCD2) often report significant issues with glare and halos from oncoming headlights. Studies show this can shorten the distance at which you can detect roadside hazards, creating a serious safety concern. Notably, these driving impairments can exist even if standard vision tests show you have 20/20 vision. If you are experiencing difficulty driving, it is crucial to discuss these specific symptoms with your ophthalmologist, as treatments may be available to resolve glare and improve your safety on the road.
How serious is macular dystrophy?
Macular dystrophy is a serious genetic eye condition that causes progressive deterioration of the macula, the part of your retina essential for clear, detailed central vision. This damage leads to the loss of central and color vision, which can significantly interfere with daily tasks like reading, driving, and recognizing faces. While the severity and rate of vision loss vary depending on the specific type of dystrophy, the condition can lead to legal blindness in some cases. Although most individuals retain their peripheral (side) vision, the seriousness of macular dystrophy is underscored by the fact that there is currently no proven cure for the condition.
What is the difference between dystrophy and degeneration?
While often used together, dystrophy and degeneration describe different concepts. Dystrophy refers to a group of inherited genetic disorders characterized by the defective development and maintenance of a specific tissue, like muscle or nerve tissue. The problem originates from a faulty gene that impacts the proteins needed for that tissue's health and structure. Degeneration , on the other hand, is the subsequent process of deterioration, where the affected tissue breaks down, weakens, and loses its function over time. In short, a dystrophy is the primary genetic disease , while degeneration is the progressive cellular damage that occurs as a result of that disease. Therefore, while degeneration is a key feature of all dystrophies, it can also occur from other causes like aging or injury, which are not themselves dystrophies.
How fast does macular dystrophy progress?
The rate at which macular degeneration progresses varies widely among individuals and depends significantly on the type of the disease. Dry macular degeneration, which is the most common form, typically advances slowly over many years, and some people may never experience significant vision loss. In contrast, wet macular degeneration is less common but can cause a rapid and severe loss of central vision, with symptoms developing over just a few days. Studies show that the annual rate of progression to the advanced wet form is approximately 3.2 per 100 people with early or intermediate stage disease, while the rate for progression to the advanced dry form (geographic atrophy) is about 2.0 per 100 people. This wide range in progression speed, from years to mere days, highlights the importance of regular eye exams for monitoring.
Can glasses help macular dystrophy?
While standard prescription glasses cannot correct the central vision loss caused directly by macular dystrophy, they are often a crucial part of managing the condition. Many people with macular dystrophy also have a separate refractive error, such as nearsightedness, farsightedness, or astigmatism. By correcting these issues, glasses ensure the sharpest possible image is focused onto the retina, which helps you maximize your remaining peripheral and side vision. For more targeted support, your eye doctor may recommend specialized low-vision aids that can be mounted onto eyeglass frames. These tools, including magnifiers, high-powered reading lenses, or telescopic systems, can significantly improve your ability to perform tasks like reading, writing, or recognizing faces.
How serious is corneal dystrophy?
The seriousness of corneal dystrophy is highly variable and depends entirely on the specific type of the condition. Many individuals are affected so mildly that they experience no symptoms for their entire lives or notice only slow, gradual changes over many decades. For others, the condition can be more severe, causing significant discomfort, painful corneal erosions, and a progressive decline in vision that eventually interferes with daily activities. While there is no cure for the underlying genetic causes, even the most serious cases that lead to significant vision loss can often be managed effectively with treatments like corneal transplants, which are highly successful at restoring sight.