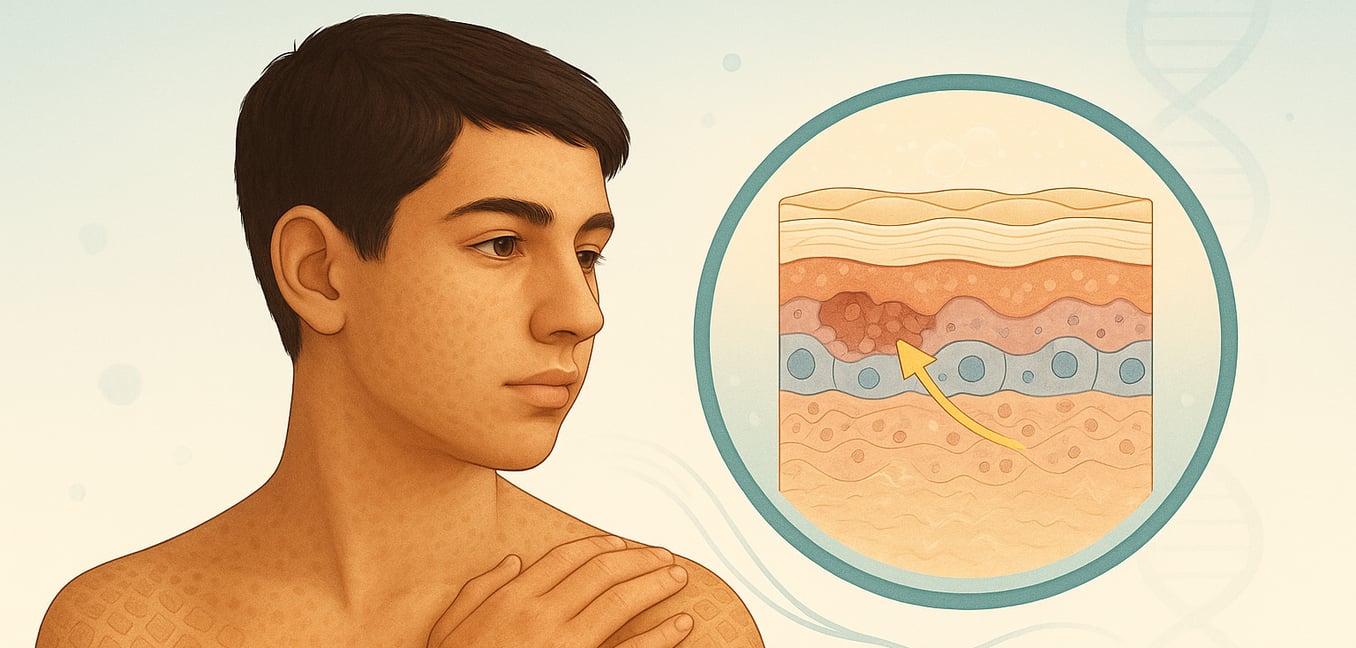
X-linked ichthyosis (XLI) is an inherited genetic disorder that primarily affects males, causing the skin to become persistently dry and scaly. As the second most common form of ichthyosis, its signs can vary significantly from person to person. While it is a lifelong condition, symptoms may not be apparent at birth, typically developing within the first few weeks or months of life. The condition results from a deficiency of an enzyme called steroid sulphatase, which disrupts the normal process of shedding dead skin cells and can lead to other associated health issues. Understanding its range of symptoms is crucial for accurate diagnosis and comprehensive care.
The most prominent symptom of XLI is the development of scales on the skin. These scales are often brownish or dark, rhombic (diamond-shaped), and can give the skin a "dirty" or "unwashed" appearance. They may appear all over the body but are most commonly found on the trunk, the back of the neck, and the outer surfaces of the arms and legs. In contrast, the major body folds, like the creases behind the knees and in the elbows, are often spared, as are the palms of the hands and soles of the feet. The severity of the scaling can fluctuate, frequently worsening in the cold, dry weather of winter and improving, or even temporarily resolving, during the summer months. While most boys develop these characteristic scales by their first birthday, some newborns may show a mild, transient scaling that fades before reappearing later in childhood.
Beyond the visible skin changes, XLI can be associated with several other conditions, which are known as extracutaneous manifestations. It is important for individuals and their families to be aware of these potential symptoms, as they may require monitoring or treatment by different specialists. Not every person with XLI will experience these, but common associated findings include:
- Harmless, cloudy spots in the eyes, called corneal opacities, which develop in about half of adult males but do not affect vision.
- An increased risk of undescended testicles (cryptorchidism), occurring in up to 20% of boys with the condition.
- A higher likelihood of neurodevelopmental conditions, with studies showing an increased risk for attention-deficit hyperactivity disorder (ADHD) and autism spectrum disorder.
- Difficult or prolonged labor for female carriers of the condition, due to the enzyme deficiency affecting the placenta. In rare cases, when a larger section of the X chromosome is affected, XLI can be part of a "contiguous gene syndrome," leading to additional issues like delayed growth or intellectual development. The visible nature of the scaling can also have a significant psychological impact, sometimes leading to social challenges and self-confidence issues, particularly during school years.
What does ichthyosis skin look like?
Ichthyosis is characterized by dry, scaly skin that often has a distinctive “fish scale” appearance, which is where the condition gets its name. These scales can vary significantly in size, texture, and color, ranging from fine, white, or gray flakes to larger, darker, and thicker plates that may appear stuck to the skin. The color of the scales often corresponds to a person’s natural skin tone, with darker skin typically having darker scales. Affected skin often feels rough, and in some forms of ichthyosis, it can also appear red, tight, or develop warty-like ridges, particularly in skin creases. It is common for the natural lines on the palms of the hands and soles of the feet to look more prominent and develop painful cracks, especially in dry weather.
Can people with ichthyosis get tattoos?
Getting a tattoo with ichthyosis is a complex decision that carries significant risks and requires careful medical consideration. Because ichthyosis compromises the skin’s natural barrier and healing processes, the tattooing procedure can lead to a higher likelihood of infection, poor healing, and potential scarring. The constant scaling and shedding of skin may also affect how the ink is retained, possibly causing the tattoo to fade, blur, or appear uneven over time. Before considering a tattoo, it is crucial to consult with your dermatologist. They can assess the severity and type of your ichthyosis to advise on the potential risks and determine if it is a safe option for your specific condition.
How do you test for X-linked ichthyosis?
Diagnosing X-linked ichthyosis is confirmed through a combination of biochemical and genetic tests, typically requested by a specialist following a clinical examination. The primary genetic test is a chromosomal microarray analysis, which uses a blood sample to effectively identify the large deletions in the STS gene responsible for most cases. If this test is negative but clinical suspicion remains high, DNA sequencing of the STS gene can be performed to detect smaller deletions or point mutations that a microarray might miss. Additionally, a diagnosis can be supported by biochemical tests that measure the activity of the steroid sulfatase enzyme in cultured skin cells, a method that is highly sensitive for detecting a loss of function from any type of mutation.
Can ichthyosis be detected before birth?
Yes, it is possible to detect certain types of ichthyosis before birth, particularly the more severe forms. Prenatal ultrasound scans, especially during the second or third trimester, can reveal characteristic physical signs such as abnormal facial features, a persistently open mouth, fixed limbs, and echogenic amniotic fluid. For families with a known history of ichthyosis or when ultrasound findings are suspicious, a definitive diagnosis can be made through genetic testing. This involves analyzing fetal DNA obtained from procedures like amniocentesis or chorionic villus sampling to identify the specific gene mutations responsible for the disorder, such as those in the ABCA12 gene for Harlequin ichthyosis. A confirmed prenatal diagnosis is critical for genetic counseling and preparing for the specialized medical care the infant will require immediately after birth.
How do you treat inherited ichthyosis?
Since there is no cure for inherited ichthyosis, treatment is a lifelong process focused on managing symptoms like dry skin and scaling. The foundation of care is a consistent daily routine that includes bathing or soaking to hydrate the skin and soften scale, which can then be gently removed with a soft washcloth or pumice stone. To lock in this moisture, a specialized moisturizer containing an active ingredient like urea, lactic acid, or glycolic acid should be applied to damp skin within minutes of bathing. For more severe cases, a dermatologist may prescribe medications such as powerful topical or oral retinoids to reduce significant hyperkeratosis. Managing related issues like deep cracks with petroleum jelly and promptly treating any secondary skin infections are also critical components of a comprehensive treatment plan.
What is the difference between ichthyosis and eczema?
The primary difference between ichthyosis and eczema lies in their fundamental cause and appearance. Ichthyosis is a genetic disorder characterized by a defect in the skin's natural shedding process, leading to a chronic buildup of thick, dry, fish-like scales. In contrast, eczema (atopic dermatitis) is an inflammatory condition driven by an overactive immune response, which causes symptoms like redness, intense itching, and weeping rashes. While both involve a compromised skin barrier, the key distinction is that ichthyosis is a primary disorder of scaling, whereas eczema is a primary disorder of inflammation. However, the defective barrier in ichthyosis, particularly ichthyosis vulgaris, is a major risk factor for developing eczema because it allows allergens to more easily penetrate the skin and trigger an immune reaction.
How does x-linked recessive inheritance work?
X-linked recessive inheritance occurs when a disorder is caused by a genetic mutation on the X chromosome. Because males (XY) have only one X chromosome, they will be affected if they inherit just a single copy of the mutated gene from their mother. In contrast, females (XX) have two X chromosomes and must inherit two copies of the mutated gene—one from each parent—to display the condition. A female who inherits only one mutated copy is considered a "carrier"; she typically shows no symptoms because her healthy X chromosome compensates, but she has a 50% chance of passing the faulty gene to her children. This inheritance pattern explains why conditions like hemophilia and Duchenne muscular dystrophy are significantly more common in males.