An Introduction to Recessive X-Linked Ichthyosis
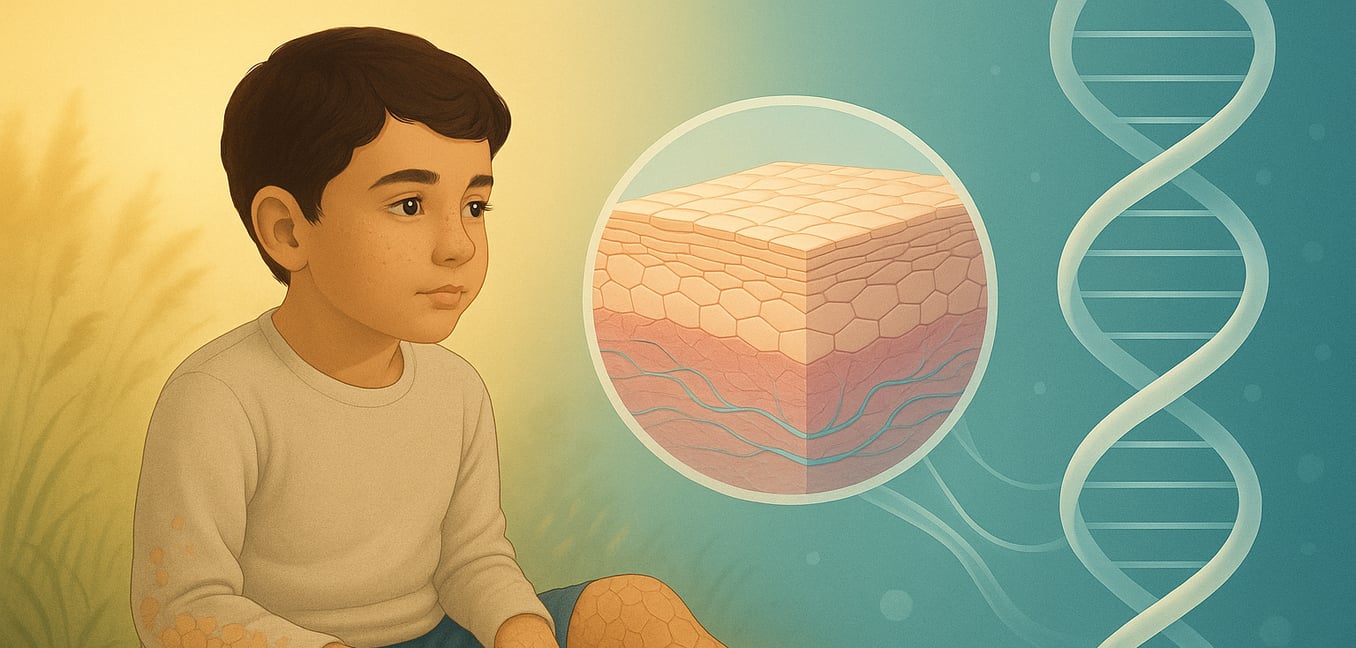
Recessive X-linked ichthyosis (XRI) is a genetic skin condition that almost exclusively affects males, making it the second most common inherited ichthyosis. It is caused by a deficiency of an enzyme called steroid sulfatase (STS). This enzyme shortage disrupts the skin’s natural shedding process, causing old skin cells to accumulate and form the condition's characteristic scales.
While the severity can vary, XRI has a consistent baseline presentation. Symptoms typically appear within the first few months of life. Affected boys develop large, polygonal, plate-like scales that are often dark brown or grayish, sometimes creating a "dirty" appearance on the skin. These scales are most noticeable on the neck, trunk, and the front of the legs and back of thearms. The palms, soles, and the creases of the elbows and knees are characteristically spared. Unlike many other skin conditions, itching is usually mild or absent.
XRI is more than just a skin disorder. Even in its most common form, it is associated with a set of non-skin features:
- Corneal Opacities: About half of affected males develop tiny, dot-like specks on the cornea of their eyes. These are harmless, do not affect vision, and are typically only visible during an eye exam.
- Cryptorchidism: Up to 20% of boys with XRI are born with undescended testicles. This requires medical monitoring due to potential effects on fertility and a slightly increased risk of testicular cancer later in life.
- Neurodevelopmental Links: There is a well-established connection between XRI and a higher likelihood of developing conditions like attention-deficit hyperactivity disorder (ADHD) and autism spectrum disorder.
- Obstetric Complications: The STS enzyme deficiency in the placenta during pregnancy can lead to low maternal estriol levels on prenatal tests and may be linked to prolonged or difficult labor.
The Primary Driver of Variation: Genetics
The root cause of XRI is always a faulty steroid sulfatase (STS) gene on the X chromosome. However, the exact nature of this genetic error is the single most important factor determining whether an individual has a relatively straightforward skin condition or a complex, multi-system disorder.
Non-Syndromic XRI: The Baseline Severity
In about 10% of cases, XRI is caused by a point mutation. To use an analogy, if the genetic code is a cookbook, a point mutation is like a single typo in the recipe for the STS enzyme. This small error is enough to make the enzyme non-functional, leading to the classic symptoms of XRI described earlier.
This form is considered "non-syndromic" because the genetic mistake is confined to the STS gene. Individuals experience the characteristic skin scaling and have the associated risks for corneal opacities, cryptorchidism, and neurodevelopmental conditions like ADHD, but they do not have the additional severe features seen in other forms of the disorder.
Syndromic XRI: The Impact of Contiguous Gene Deletions
In up to 90% of cases, the cause is not a small typo but a complete deletion of the STS gene. Returning to our cookbook analogy, this is like ripping an entire page out of the book. If that page only contained the STS recipe, the outcome is the same as a point mutation.
However, these deletions are often larger, removing a whole segment of the chromosome that includes neighboring genes. This is known as a contiguous gene deletion syndrome, and it dramatically expands the clinical picture. The resulting symptoms depend entirely on which "recipes" were on the ripped-out page. This transforms XRI from a skin condition into a complex disorder requiring a multidisciplinary approach to care. The specific features are directly tied to the functions of the co-deleted genes.
For example, if the deleted segment includes:
- A gene responsible for the sense of smell and puberty ( KAL1 ), the individual may also have Kallmann syndrome.
- A gene that regulates bone growth ( SHOX ), it can lead to a condition causing short stature and a specific wrist deformity.
- Genes involved in brain function ( VCX3A or NLGN4X ), it can result in more significant intellectual disability and communication challenges than the baseline risk associated with XRI.
Secondary Modulators of Severity
While the type of genetic error sets the primary course for XRI, other factors can fine-tune the severity of its symptoms, particularly the skin condition. An individual's experience with XRI is shaped by their age, their environment, and their unique genetic background.
The Role of Age
The intensity of XRI often follows a predictable path through life. After emerging in the first few months, the condition typically reaches its peak during childhood and adolescence. The large, dark scales can be most prominent and socially challenging during these years. However, many individuals find that their skin symptoms gradually become less severe as they enter adulthood, making the condition easier to manage over time.
The Influence of Environment and Co-existing Genetics
The external environment plays a powerful role in the day-to-day management of XRI. Cold, dry air, especially in winter, draws moisture from the already compromised skin barrier, making the scaling tighter, drier, and more pronounced. Conversely, many people experience a significant improvement in warm, humid weather. Sun exposure, in particular, has been noted to have a remarkable, though temporary, clearing effect on the scales for some individuals.
Finally, an individual’s broader genetic makeup can influence the severity of the skin symptoms. A key example is the interaction with the filaggrin ( FLG ) gene, which is known to cause another common dry skin condition, ichthyosis vulgaris. If a person with XRI also inherits a faulty FLG gene, this genetic "double hit" can disrupt the skin barrier even further, often leading to a much more severe skin condition than would be expected from the STS gene defect alone.