Beyond Transplants: The Future of Treating Fuchs' Corneal Dystrophy
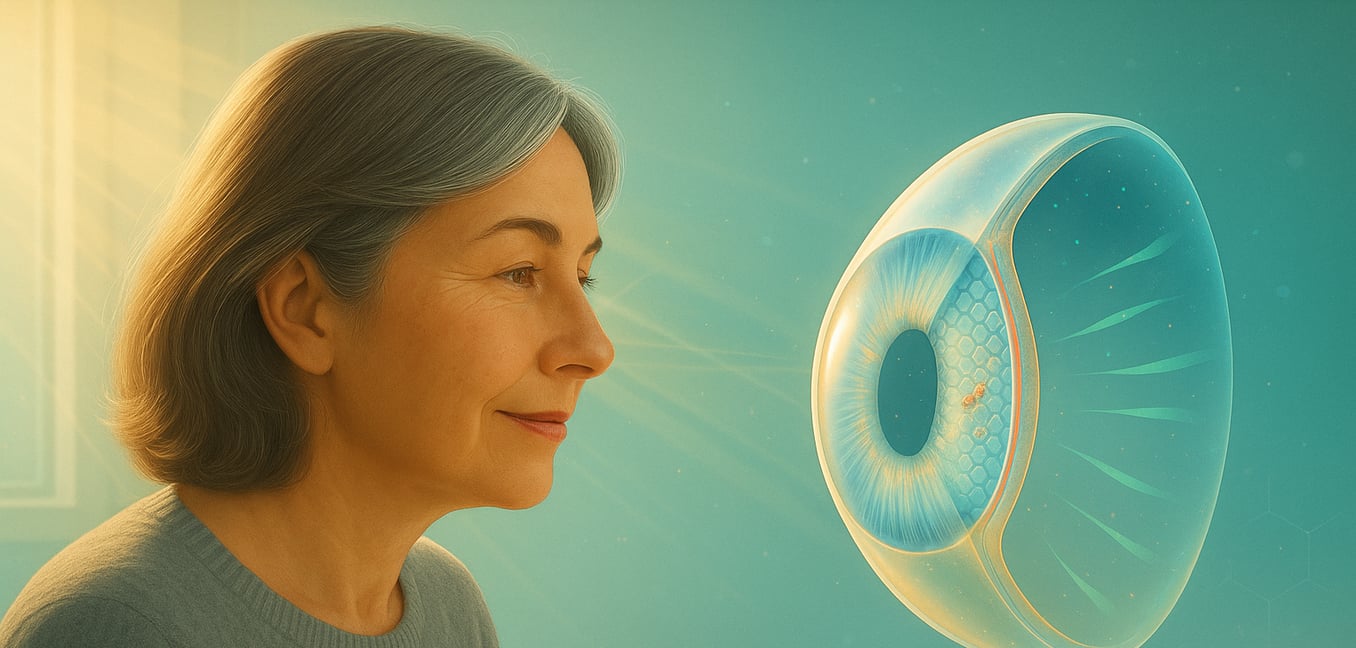
Fuchs' endothelial corneal dystrophy is an inherited eye disease affecting the cornea—the clear, dome-shaped window at the front of the eye. Often emerging after age 40, it causes a gradual, painless decline in vision. The problem originates in a single, vital layer of cells that keeps the cornea clear, and until recently, a full corneal transplant was the only definitive solution. Now, a wave of research is revolutionizing this landscape, offering new hope through smarter diagnostics, less invasive surgeries, and innovative non-surgical therapies that target the disease at its source.
The Root of the Problem: Dying Cells and a Cloudy Cornea
Vision loss in Fuchs' dystrophy stems from the failure of a specific cell layer lining the inner cornea called the endothelium. These endothelial cells act as tiny pumps, constantly removing fluid to keep the cornea thin and transparent. Crucially, these cells do not regenerate; the number you have at birth is all you will ever get.
In Fuchs' dystrophy, these cells die off prematurely. As the cell population dwindles, their pumping capacity weakens. Fluid accumulates, causing the cornea to swell and become cloudy, leading to blurred vision, glare, and halos around lights, particularly in the morning.
Recent discoveries have revealed a key reason for this accelerated cell death. Scientists found that in people with Fuchs', the endothelial cells accumulate toxic levels of iron. This excess iron acts like rust inside the cell, triggering a destructive chain reaction called oxidative stress and causing the cells to self-destruct through a process known as ferroptosis. This insight has opened the door to therapies designed to protect cells from this specific pathway of destruction.
Smarter Diagnosis and Less Invasive Surgery
The evolution in treating Fuchs' begins with a deeper understanding of an individual patient's condition, moving beyond simple observation to molecular-level analysis. This clarity is empowering less invasive procedures that leverage the body's own healing potential.
A Molecular-Level Diagnosis
A powerful new technology, single-cell RNA sequencing, is transforming diagnostics. Instead of relying on an ophthalmologist's visual assessment of corneal cloudiness, this tool can analyze the genetic activity within individual cells. It provides a detailed "report card" on cellular health, revealing precisely what percentage of cells are still healthy versus those expressing genes that drive the disease. This data-driven insight gives doctors a clear picture of disease progression and helps determine if a patient has enough healthy cells to benefit from newer, less invasive surgeries.
A Self-Healing Approach to Surgery
This improved diagnostic clarity directly enables a procedure known as Descemet stripping only (DSO). Rather than replacing the entire endothelial layer with donor tissue, as in a traditional transplant, DSO involves carefully removing only the damaged cells from the central cornea. This prompts the patient’s own healthy peripheral cells to migrate inward and repopulate the area, allowing the eye to essentially heal itself. The success of DSO hinges on having a sufficient reserve of healthy cells—a fact that can now be determined with much greater certainty. This procedure can also be enhanced with Rho kinase inhibitor eye drops, which accelerate cell migration and speed up recovery.
The Promise of Therapeutic Eye Drops
While less invasive surgery is a major step forward, the ultimate goal is to treat Fuchs' dystrophy without any surgery at all. Researchers are developing therapeutic eye drops that target the disease at its cellular and genetic roots, shifting the focus from reactive treatment to proactive prevention.
Neutralizing Cellular Damage
Building on the discovery that iron-driven cell death (ferroptosis) is a key culprit, one promising strategy aims to neutralize this damage. Researchers at the University of Iowa are developing an eye drop containing ubiquinol, the active form of Coenzyme Q10. This powerful antioxidant can be delivered directly to the cornea to restore the natural balance within the cells and shield them from oxidative stress. By protecting the existing endothelial cells, these drops could slow or halt disease progression, potentially preventing vision loss and reducing the need for future surgery.
Targeting the Genetic Source
A second, more targeted approach aims to correct the problem at its genetic origin. Design Therapeutics is developing an eye drop, DT-168, that functions as a gene-targeted therapy. It uses a small molecule designed to find and reduce the activity of the faulty TCF4 gene, which is responsible for the most common form of Fuchs'. By lowering the production of the harmful genetic material that damages corneal cells, DT-168 has the potential to restore normal cell function and stop the disease. This therapy has already advanced into clinical trials, a critical step toward a non-surgical, disease-modifying treatment.
Editing the Genetic Blueprint with Gene Therapy
While some eye drops manage gene activity, another field of research is aiming for a more permanent solution: directly editing the faulty gene itself. This approach, known as gene therapy, could one day offer a one-time cure by disabling the harmful gene at its source.
A Precise Gene-Editing Tool
Researchers at the University of Oregon’s Knight Campus are pioneering a gene therapy using the CRISPR-Cas9 tool to address a rare, early-onset form of Fuchs'. Led by Dr. Bala Ambati, the team developed a method to precisely "knock out" the mutant gene that produces a toxic protein. In animal studies, this treatment successfully stopped the loss of endothelial cells and preserved the cornea's clearing function, preventing the swelling that causes cloudy vision.
Overcoming a Cellular Hurdle
A major challenge was applying gene editing to corneal endothelial cells, which are non-dividing and do not replenish themselves. The team overcame this with a novel technique that targets the "start" signal in the gene's instructions. By disrupting this starting point, the cell's machinery can no longer "read" the instructions to build the harmful protein, effectively silencing the gene without requiring the cell to divide—a breakthrough with potential implications for other genetic diseases.
A New Generation of Cell Therapies
Beyond protecting existing cells or editing genes, a futuristic approach aims to simply replenish the cornea's depleted cell population. Injectable cell therapy represents a paradigm shift from donor tissue transplants to a one-time injection that could restore the eye's endothelial layer.
A Simple Injection to Repopulate Cells
One leading technique, developed by Aurion Biotech, involves injecting a solution of lab-grown human corneal endothelial cells into the eye. These cells are combined with a ROCK inhibitor compound that helps them adhere to the cornea and function properly. After the injection, the patient lies face-down for a few hours to allow the cells to settle into a new, healthy layer. This therapy, which can treat up to 100 patients from a single donor cornea, is already approved in Japan and is in clinical trials in the U.S.
Magnetic Guidance for Precision
An even simpler method from Emmecell uses magnetic nanoparticles to guide injected cells into place. Lab-grown endothelial cells are made magnetic before being delivered to the clinic. The treatment is a simple injection performed in an ophthalmologist's office, without an operating room. Afterward, a magnetic eye patch is worn for a short time, using a gentle magnetic field to pull the new cells into a single, functional layer. This approach dramatically simplifies the procedure and recovery, allowing patients to resume normal activities almost immediately.