Preventing Amish Lethal Microcephaly
Amish Lethal Microcephaly (MCPHA) is a devastating genetic disorder found within the Amish community of Pennsylvania. Characterized by a severely small head at birth and profound developmental issues, the condition is uniformly fatal, with infants rarely surviving past their first year. Because there is no cure or effective treatment for MCPHA, the only available strategy for families and the community is prevention, which is made possible through modern genetic science.
This article focuses on the key strategies for preventing this heartbreaking disorder, grounded in an understanding of its genetic roots.
Understanding the Cause: The Genetic Basis of MCPHA
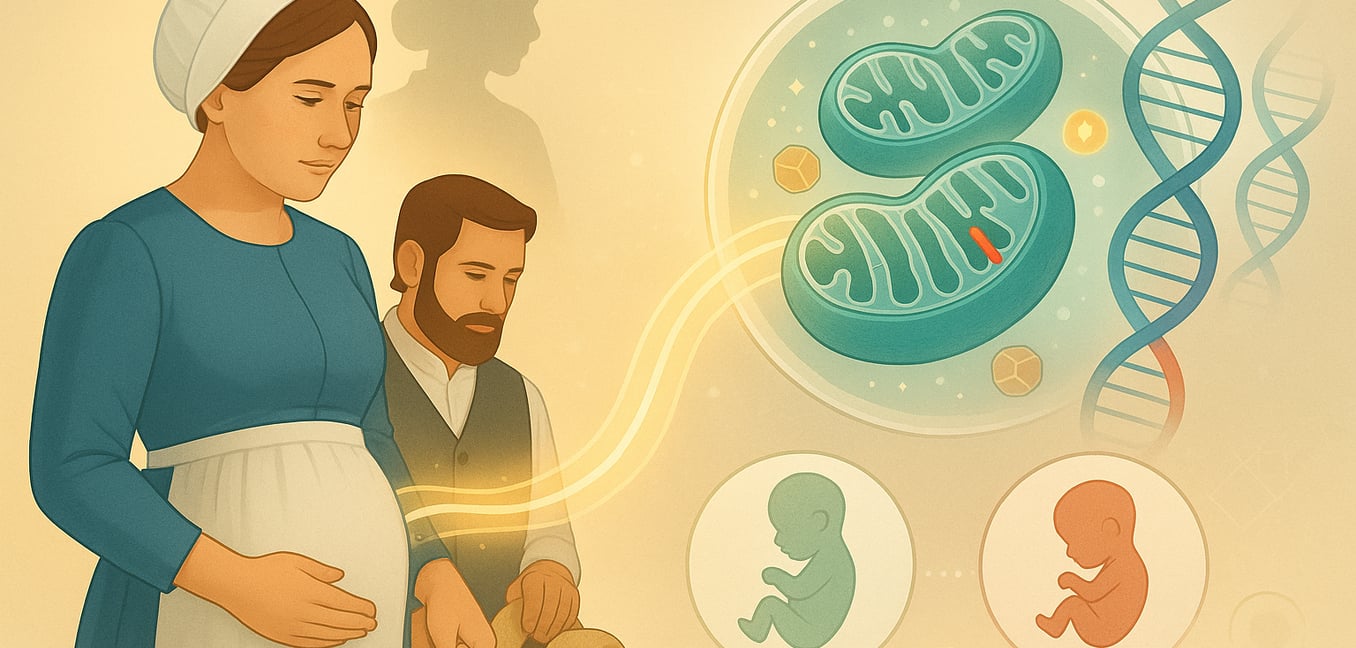
To understand how MCPHA can be prevented, one must first understand its cause. The disorder is not caused by an infection or environmental factor, but by an error in a single gene. This type of condition is known as autosomal recessive, meaning a child must inherit a non-working copy of the specific gene from both parents to be affected.
The gene responsible for MCPHA is SLC25A19 . Its job is to provide the instructions for building a special transporter protein. This protein acts like a gatekeeper for the mitochondria, which are the tiny powerhouses inside our cells. Specifically, it transports thiamine pyrophosphate (TPP), the active form of vitamin B1, into the mitochondria.
Inside the mitochondria, TPP is essential for converting food into energy. Without the transporter, TPP cannot enter, and the cell's energy production line grinds to a halt. This energy crisis is particularly catastrophic for the developing brain, which requires immense amounts of energy to grow properly in the womb. The result is severe disruption of brain formation, leading to the features of MCPHA.
The Cornerstone of Prevention: Genetic Counseling and Carrier Screening
Since MCPHA is a recessive condition, a person can carry one non-working copy of the SLC25A19 gene and be perfectly healthy. These individuals are known as "carriers." The risk of having an affected child only arises when two carriers have children together. For each pregnancy, such a couple has a one-in-four (25%) chance of having a child with MCPHA.
Genetic counseling and carrier screening are the most powerful tools available to help individuals understand their risk and make informed decisions about family planning.
The Role of Genetic Counseling
Genetic counseling provides essential support and information. In a confidential session, a genetic counselor can explain the inheritance pattern in detail, helping families understand the biological basis of the condition. For parents who have already had an affected child, this process can help alleviate feelings of guilt and provide a safe space to discuss the emotional impact and consider options for future pregnancies. This guidance is a cornerstone of family-centered care, empowering parents with knowledge during an incredibly difficult time.
Community Carrier Screening
Within a founder population like the Amish community, where the carrier frequency for this specific genetic variant is higher, community-wide carrier screening is a highly effective public health initiative. This involves offering a simple genetic test, often from a blood or saliva sample, to any adult who wishes to know their carrier status.
By identifying carriers proactively, this approach allows individuals to learn about their genetic risks before marriage or starting a family. When implemented in a culturally sensitive manner, in partnership with local clinics and community leaders, carrier screening can significantly reduce the incidence of the disorder by giving couples the information they need to plan for a healthy family.
Reproductive Options for Carrier Couples
When both partners in a couple are identified as carriers of the SLC25A19 mutation, they have several reproductive options that can prevent the birth of a child with MCPHA. The choice among these options is deeply personal and depends on a couple's ethical, religious, and personal values.
- Prenatal Diagnosis: Testing the fetus during pregnancy through procedures like amniocentesis or chorionic villus sampling (CVS) to determine if it has inherited the two non-working genes.
- Preimplantation Genetic Testing (PGT): This option is used with in vitro fertilization (IVF). Embryos are created and tested for the disorder before being transferred to the uterus, allowing parents to select an unaffected embryo for implantation.
- Using a Donor: Utilizing donor sperm or a donor egg from an individual who is confirmed not to be a carrier of the gene mutation eliminates the risk of passing on the condition.
Appendix: Clinical Features, Diagnosis, and Management
While prevention is the primary focus, it is helpful to understand the clinical details of Amish Lethal Microcephaly for context.
Clinical and Diagnostic Features
Infants with MCPHA are born with profound microcephaly, meaning their head circumference is exceptionally small, often four to twelve standard deviations below the average. They have distinct facial features, including a sloping forehead. Neurological signs are severe and include myoclonic seizures (brief, shock-like jerks), low muscle tone in the torso, and stiff limbs.
Brain scans, such as an MRI, reveal the devastating impact on the brain's structure. Common findings include lissencephaly, where the brain's surface is abnormally smooth instead of folded, and an underdeveloped or missing corpus callosum, the bundle of nerves that connects the two halves of the brain.
Laboratory tests provide biochemical confirmation. Blood tests often show high levels of lactic acid, while urine tests reveal elevated levels of alpha-ketoglutaric acid. These are direct chemical signatures of the stalled energy pathway in the cells. However, a definitive diagnosis is made through genetic testing that identifies the specific mutation in the SLC25A19 gene.
Management and Prognosis
There is no cure for MCPHA. Medical care is palliative, meaning it is focused on providing comfort and managing symptoms rather than attempting to cure the underlying condition. Anticonvulsant medications may be used to control seizures, and feeding tubes are often necessary to provide nutrition.
It is important to note that unlike related disorders, high-dose thiamine (vitamin B1) supplements are ineffective. The genetic defect causes a complete loss of the transporter protein, so even with extra thiamine in the body, it cannot get into the mitochondria where it is needed.
The prognosis is uniformly grim, and the condition is considered lethal. Survival is typically limited to the first few months of life. Therefore, care is centered on alleviating suffering, maximizing the infant's comfort, and providing comprehensive emotional and practical support to the family.