Emerging Technologies in Diagnosing Corneal Dystrophy
Corneal dystrophy is a group of inherited eye conditions where abnormal material accumulates in the cornea, the clear front surface of the eye. One of the most common types, Fuchs endothelial corneal dystrophy (FECD), involves the progressive loss of cells in the cornea’s innermost layer, the endothelium. These cells are essential for maintaining corneal clarity. Their decline leads to swelling, cloudiness, and vision loss, making precise diagnostic imaging critical for effective management.
Foundational Diagnostic Imaging
Ophthalmologists rely on several core imaging techniques to monitor the structural changes caused by corneal dystrophies. These tools provide a foundational understanding of the disease's impact on the cornea's layers.
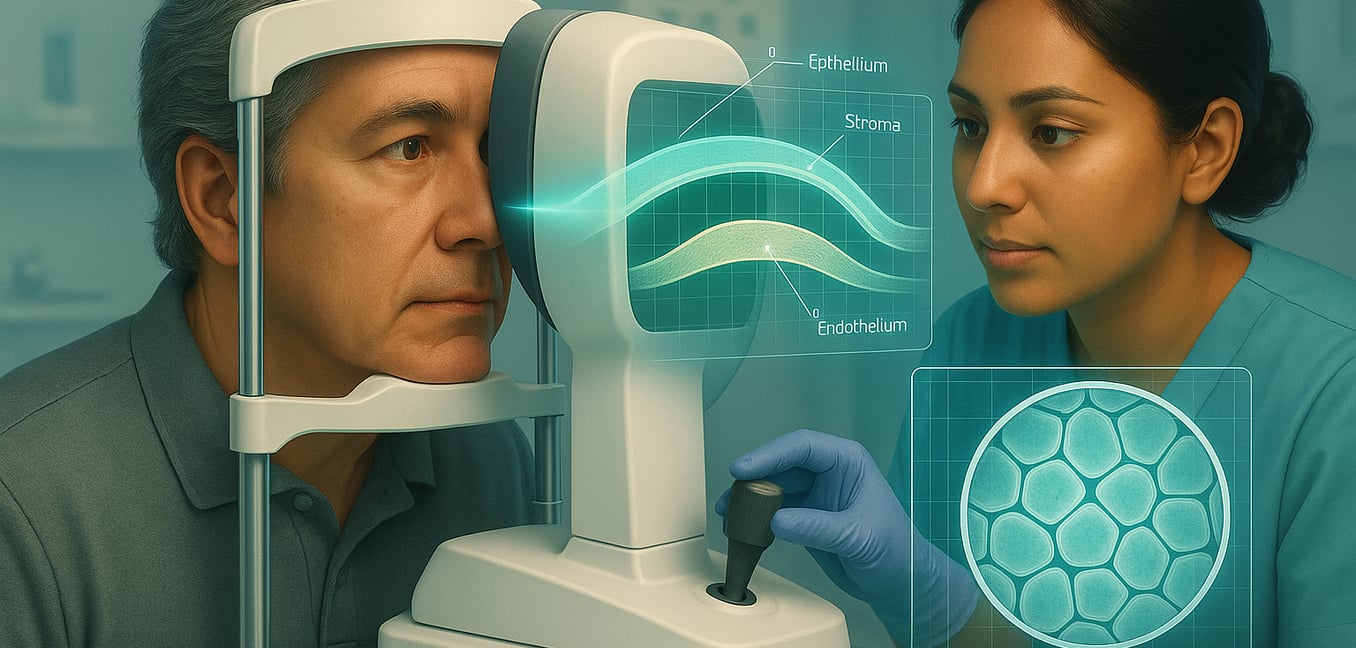
Specular Microscopy
This non-invasive photographic technique provides a magnified, direct view of the corneal endothelium. It acts as a cellular census, allowing clinicians to count endothelial cells and analyze their size and shape. In early-stage FECD, this tool is invaluable for detecting cell loss or the formation of guttae—tiny protein deposits—before they cause symptoms. However, its effectiveness diminishes in advanced cases where significant corneal swelling scatters light and obscures the view.
Anterior Segment Optical Coherence Tomography (AS-OCT)
AS-OCT functions like an optical ultrasound, using light to create a detailed, cross-sectional map of the cornea. This non-contact scan allows doctors to precisely measure the thickness of the entire cornea and its individual layers. This is crucial for detecting subtle swelling, tracking disease progression, and evaluating the cornea after transplant surgery. It is also a primary tool for monitoring the success of regenerative cell therapies, offering a real-time view of how injected cells are integrating and restoring corneal clarity.
Scheimpflug Corneal Tomography
This technology uses a rotating camera to build a comprehensive 3D map of the entire cornea. It provides detailed information on the cornea's front and back curvature, overall thickness, and any shape irregularities. This is particularly useful for detecting subtle structural changes associated with FECD, such as changes to the posterior surface, which can indicate early swelling and help predict the risk of disease progression.
Advanced High-Resolution Corneal Imaging
While foundational imaging gives a structural overview, advanced technologies offer a microscopic view of the cornea’s individual cells and tiniest structures in the living eye. These methods reveal subtle changes essential for understanding the full impact of diseases like FECD.
In Vivo Confocal Microscopy (IVCM)
IVCM acts like a high-powered microscope for the living eye, providing real-time images with cellular-level detail of all corneal layers. Its key advantage is the ability to see through corneal haze or swelling, obtaining clear views of the endothelium even in advanced cases where other methods fail. This precision is critical for guiding modern treatments. For instance, in a transplant-free procedure called Descemet stripping only (DSO), doctors rely on IVCM to confirm if a patient has enough healthy peripheral cells to regenerate the cornea, making it a key tool for patient selection.
Retroillumination Photography with Digital Analysis
This accessible method uses a standard slit-lamp camera to take pictures of the cornea while bouncing light off the back of the eye, creating a silhouette effect. This backlighting makes corneal guttae stand out as distinct dark spots against an illuminated background. The true advancement lies in pairing these photos with image analysis software, often powered by artificial intelligence. These programs automatically identify, count, and measure guttae, transforming a simple photograph into a powerful quantitative tool for staging the disease and planning surgery.
The Role of Artificial Intelligence in Automated Diagnosis
Analyzing the detailed images from advanced diagnostics can be complex and time-consuming. Artificial intelligence (AI) is transforming this process by automatically interpreting images with high precision and objectivity, complementing the expertise of specialists.
Automated and Objective Staging
AI-powered systems provide a standardized, data-driven assessment of Fuchs' dystrophy, overcoming the subjectivity of manual grading. Deep learning models analyze images to differentiate between healthy and diseased corneas with an accuracy comparable to specialists, ensuring consistent monitoring and informing decisions about the timing of surgery.
Early Disease Detection
AI's greatest strength may be identifying the disease at its earliest, subclinical stages. Algorithms can detect minute structural changes within the cornea long before a patient experiences symptoms or swelling becomes obvious. This high sensitivity acts as an early warning system for at-risk patients, especially those considering cataract surgery where undiagnosed FECD can impact outcomes.
Improved Clinical Efficiency
AI automates the labor-intensive process of analyzing corneal scans, processing images in a fraction of the time it takes a human. This streamlines the clinical workflow, potentially reducing patient wait times and allowing specialists to dedicate more time to treatment planning and patient care.
Genetic Frontiers: Gene-Based and Cellular Diagnostics
While imaging shows what is happening to the cornea, genetic diagnostics explain why it is happening at a molecular level. Identifying the underlying genetic cause is a crucial step toward personalized medicine, paving the way for diagnostics that can predict disease course and guide future treatments.
Pinpointing the Genetic Cause
From a simple blood or saliva sample, modern genetic testing can analyze a panel of genes known to cause corneal dystrophies. For FECD, this can identify a specific mutation, such as a common genetic marker responsible for most late-onset cases. This genetic confirmation provides a definitive diagnosis and valuable information about potential disease progression. This genetic fingerprint does more than confirm a diagnosis; it provides the exact target for future gene therapies designed to correct the disease at its root cause.
Lab-Based Disease Modeling
Revolutionary tools like CRISPR gene editing and induced pluripotent stem cells (iPSCs) are transforming how corneal dystrophies are studied. Scientists can use these methods to create highly accurate "disease in a dish" models from a patient's own cells. By creating or correcting the genetic flaws in these lab-grown corneal cells, researchers can pinpoint how a mutation leads to cell death. This allows them to test the effectiveness of potential new drugs or gene therapies on cells that are a perfect genetic match for the patient, a critical step before human trials.