Understanding Corneal Dystrophy
Corneal dystrophy is a group of rare, inherited disorders that cause the cornea—the transparent front surface of the eye—to become cloudy. This cloudiness results from an abnormal buildup of material in one or more of its layers. These conditions are typically non-inflammatory, progress slowly, and affect both eyes symmetrically. Importantly, they are not caused by external factors like injury or systemic disease, which helps distinguish them from more common corneal degenerations related to aging or environmental stress.
To diagnose these conditions, clinicians classify them based on the affected corneal layer (anatomic classification) or, increasingly, by their underlying genetic cause. This modern genetic approach organizes dystrophies based on their link to a specific, identified gene, while for others, the connection is still under investigation. Understanding that these are hereditary conditions is the first step in the diagnostic journey.
The Cornerstone of Detection: The Slit-Lamp Examination
The most fundamental tool for detecting corneal dystrophy is the slit-lamp biomicroscope. It provides a highly magnified, three-dimensional view of the eye, allowing a clinician to identify the tell-tale signs of a specific dystrophy and pinpoint the exact corneal layer affected. A skilled examiner can manipulate the light source, using techniques like retroillumination—bouncing light off the back of the eye—to make subtle opacities or textures stand out. These physical clues are often the first indication that a genetic condition is at play.
Epithelial and Subepithelial Findings
When the front layers of the cornea are involved, the slit-lamp reveals distinct patterns. In Epithelial Basement Membrane Dystrophy (EBMD), the most common type, an eye doctor may see faint, gray map-like outlines, tiny dot-like cysts, or delicate, swirling "fingerprint" lines. These signs represent an abnormal basement membrane that can lead to painful recurrent corneal erosions. In other dystrophies like Meesmann dystrophy, the exam instead shows countless tiny, clear bubbles scattered across the surface.
Stromal Deposit Patterns
Dystrophies affecting the stroma, the thick middle layer, are defined by the pattern of abnormal deposits. Granular Dystrophy, for example, presents with distinct, well-defined "breadcrumb" or "snowflake" opacities with clear corneal tissue between them. In contrast, Lattice Dystrophy is identified by fine, branching, glass-like lines that interlace to form a delicate lattice structure. Macular Dystrophy, the most severe of these three, causes a diffuse, ground-glass cloudiness that extends across the entire cornea, along with poorly defined gray-white spots.
Endothelial Layer Clues
Changes in the endothelium, the cornea’s deepest cell layer, often lead to corneal swelling. In Fuchs' Endothelial Corneal Dystrophy, the slit-lamp reveals characteristic drop-like bumps called guttae on the back surface of the cornea, which can create a "beaten metal" appearance. These guttae are signs of endothelial cell loss. As these pump cells fail, fluid builds up, causing corneal edema (swelling) that gives the cornea a hazy, thickened look, often resulting in blurry vision that is worse upon waking.
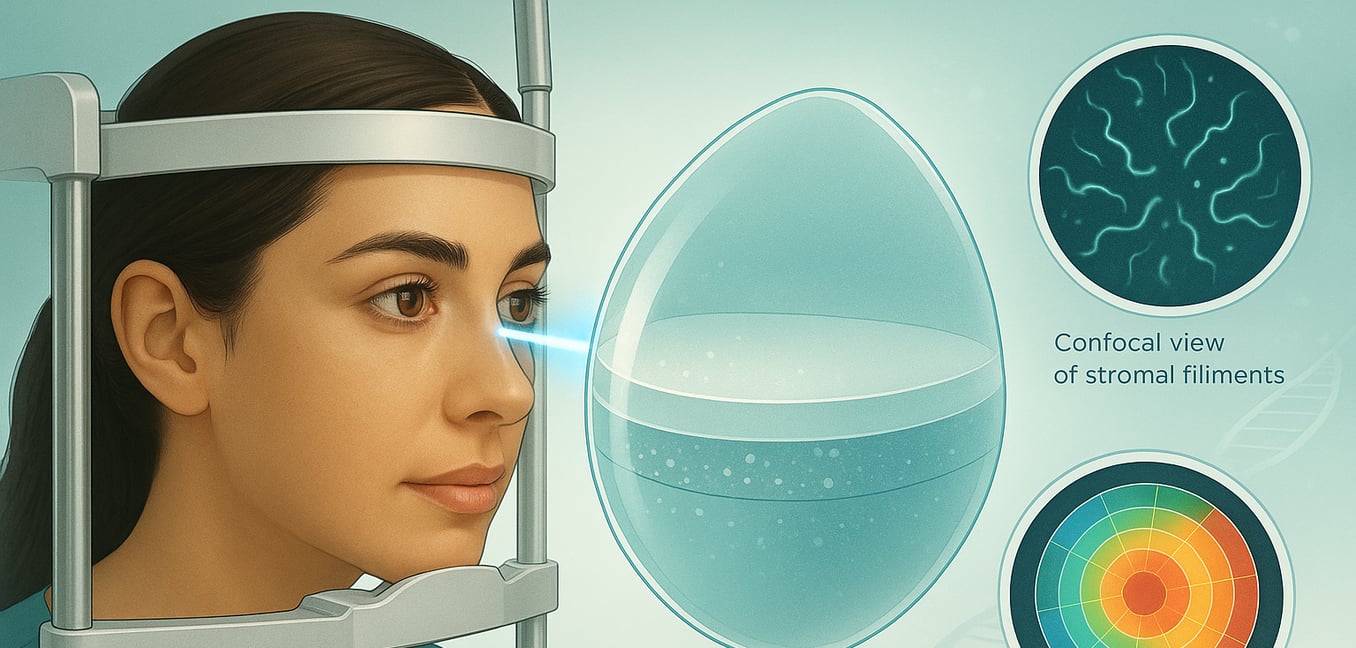
Beyond the Slit-Lamp: Advanced Diagnostic Imaging
When a slit-lamp exam suggests a corneal dystrophy, eye care professionals can turn to advanced technologies for a more detailed look. These powerful tools provide definitive answers by peering into the cornea's microscopic structure, helping to confirm a diagnosis, track progression, and plan treatment.
Confocal Microscopy: An Optical Biopsy
Confocal microscopy provides a non-invasive, high-powered view of the cornea at the cellular level. This "optical biopsy" allows clinicians to see individual cells and the specific nature of abnormal deposits without needing a tissue sample. For instance, it can visualize the fine, curly filaments in Thiel-Behnke dystrophy or the abnormal endothelial cells in Posterior Polymorphous Dystrophy. This detailed view is invaluable for differentiating between dystrophies that may appear similar on a slit-lamp exam.
Corneal Tomography: A 3D Blueprint
Corneal tomography creates a comprehensive 3D map of the entire cornea, measuring its thickness, curvature, and the shape of its front and back surfaces. This technology is crucial for managing endothelial dystrophies like Fuchs', as it can detect the earliest signs of corneal swelling long before it becomes visible during a standard exam. By precisely tracking changes in corneal thickness over time, tomography helps clinicians quantify disease progression and determine the optimal timing for surgical intervention, such as a corneal transplant.
Confirming the Diagnosis: The Genetic Link
Because corneal dystrophies are inherited, a patient's genetic background is central to the diagnostic process. Investigating family history and using modern genetic testing can move a diagnosis from a suspicion to a certainty, providing clarity for patients and their families.
Uncovering Clues in Family History
A thorough family health history is a crucial first step. Many dystrophies follow an autosomal dominant inheritance pattern, meaning an affected person has a 50% chance of passing the condition to each child. A clinician may recommend examining close relatives, as finding similar corneal changes—even if mild or asymptomatic—can help confirm a diagnosis. It is useful to ask relatives about general issues like blurry vision, eye discomfort, or a history of "weak corneas," as they may have an undiagnosed condition.
Genetic Testing for a Definitive Answer
Genetic testing offers the most definitive diagnosis by analyzing a patient's DNA for the specific mutations known to cause these disorders. While imaging reveals the physical results of a dystrophy, a genetic test identifies its root cause. This is especially valuable when symptoms overlap between different conditions, such as the various stromal dystrophies linked to the TGFBI gene. A simple blood or saliva sample can pinpoint the exact genetic error, confirming the specific type of dystrophy and ending any diagnostic uncertainty.
The Role of Genetic Counseling
Receiving a genetic diagnosis is often followed by genetic counseling. This supportive process helps you understand the results in a personal context. A genetic counselor explains the inheritance pattern of your condition and discusses the implications for family planning and the potential risk for your children or other relatives. This guidance empowers you to make informed decisions and helps family members understand if they should also consider screening, turning a diagnosis into a tool for proactive health management.