New Imaging Techniques for Detecting Neuroblastoma
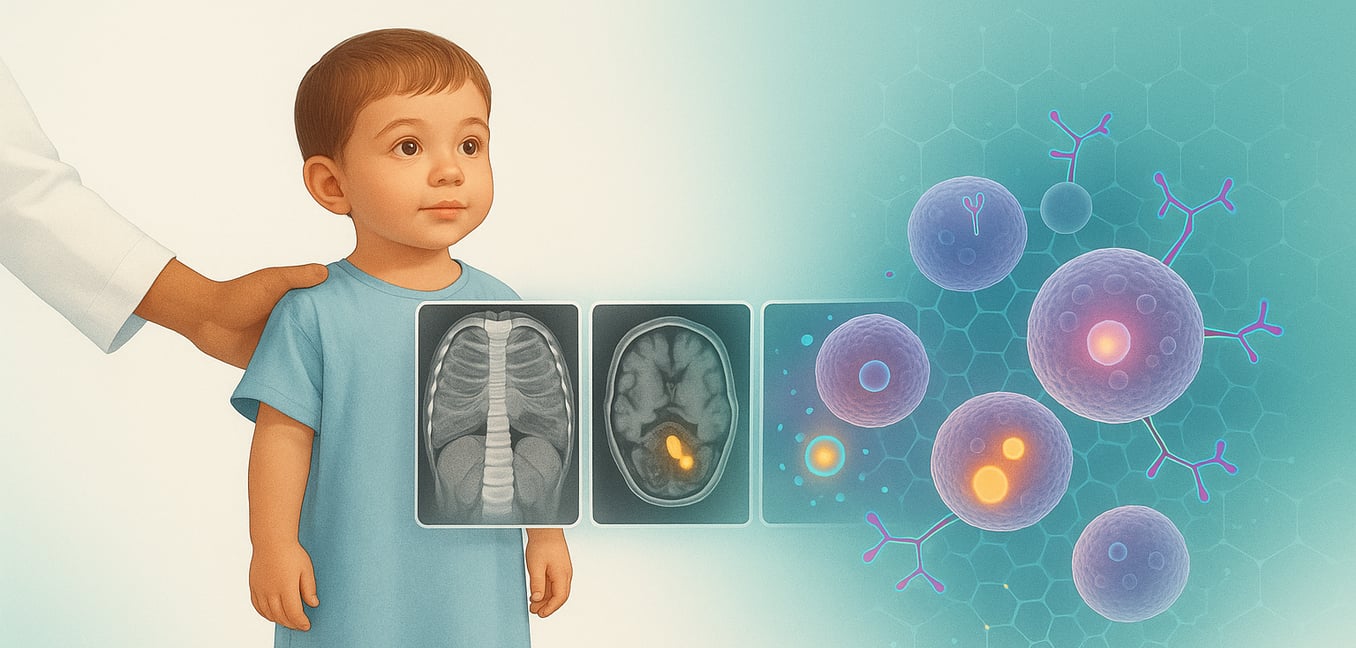
Neuroblastoma is a rare childhood cancer that develops from immature nerve cells called neuroblasts. As a remnant of fetal development, these cells typically mature or disappear after birth, which is why this cancer almost exclusively affects infants and young children. Tumors most often form in the adrenal glands atop the kidneys but can appear anywhere along the sympathetic nervous system in the abdomen, chest, or neck. Neuroblastoma is uniquely unpredictable; some tumors in infants may disappear on their own, while others can be highly aggressive and spread quickly. This variability makes accurate diagnosis and staging, powered by medical imaging, critical for determining the right treatment path.
Before exploring new techniques, it is essential to understand the standard imaging tools used to diagnose and stage neuroblastoma. These conventional methods provide the foundational anatomical picture of the tumor. An Ultrasound (US) is often the first step, using sound waves to confirm if a lump is a solid mass. A Computed Tomography (CT) scan then offers detailed cross-sectional images, defining the tumor's size and its relationship to nearby organs and blood vessels. Finally, Magnetic Resonance Imaging (MRI) excels at visualizing soft tissues without radiation, making it ideal for assessing tumors near the delicate spinal cord. While vital, these scans primarily show structure, which is why newer functional and molecular imaging techniques are so revolutionary.
Advances in Molecular Imaging: Beyond MIBG
While conventional scans show anatomy, molecular imaging reveals a tumor's biological activity, often by using Positron Emission Tomography (PET) to track specialized tracers within the body. For years, the MIBG scan was the standard for neuroblastoma, but newer, more sensitive tools are providing a clearer window into the disease.
FDG-PET Scans
This scan uses a radioactive form of sugar called FDG. Because aggressive cancer cells consume more energy than healthy cells, they absorb more of this tracer and "light up" on the scan. This technique is especially useful for identifying MIBG-negative tumors—those that do not absorb the traditional MIBG tracer—and for assessing the full extent of the disease. By providing a metabolic profile of the cancer, FDG-PET helps doctors monitor how well treatment is shutting down the tumor's energy supply.
Somatostatin Receptor Imaging
A major breakthrough involves targeting the somatostatin receptor, a protein found on the surface of many neuroblastoma cells. A tracer called DOTATATE, when used in a PET scan, binds to these receptors with exceptional precision. These DOTATATE PET scans can detect neuroblastoma lesions with remarkable clarity, often identifying spots of disease missed by MIBG. This advance also opens the door to "theranostics," a strategy where the same targeting molecule is used for both diagnosis and for delivering targeted radiation therapy directly to cancer cells.
F-DOPA PET Scans
This technique leverages the unique biology of neuroblastoma cells, which are involved in producing hormones like dopamine. F-DOPA is a radioactive version of a natural building block used in this process. By tracking where F-DOPA accumulates, doctors get a highly specific map of neuroblastoma tumors. This method often produces high-quality images with less background interference than other scans, making it easier to spot small areas of disease and proving more sensitive than MIBG for some children.
The Growing Role of Functional MRI Techniques
While traditional MRI shows a tumor's structure, functional MRI techniques add another layer of information by peering into its biology. These advanced methods reveal details about cellular makeup and activity—like water movement and blood flow—without exposing the child to ionizing radiation.
Diffusion-Weighted Imaging (DWI)
This powerful technique measures how easily water molecules move within tissues. In a densely packed tumor, water movement is restricted, making these areas stand out. DWI can therefore indicate tumor aggressiveness and provide an early sign that treatment is working. As chemotherapy kills cancer cells, they break apart, allowing water to move more freely—a change DWI can detect long before the tumor visibly shrinks.
Dynamic Contrast-Enhanced (DCE) MRI
DCE-MRI provides a detailed look at a tumor's blood supply. After a contrast agent is injected, the scanner tracks how it flows through the tumor's blood vessels. This reveals how leaky and disorganized the vessels are—a key indicator of tumor aggressiveness. The information is also valuable for monitoring the effectiveness of anti-angiogenic therapies, which are treatments designed to cut off a tumor's blood supply.
Blood Oxygen Level-Dependent (BOLD) MRI
This technique maps oxygen levels within a tumor by taking advantage of a simple fact: oxygen-rich and oxygen-poor blood have different magnetic properties. The scanner can detect these differences, creating a map that shows which parts of the tumor are starved for oxygen, or hypoxic. Since hypoxic areas are often more resistant to radiation and chemotherapy, BOLD MRI allows doctors to identify these stubborn pockets and potentially tailor treatments for a more effective strategy.
Emerging Horizons: Radiomics and Artificial Intelligence
Advanced imaging provides remarkable pictures, but a vast amount of data remains hidden from the human eye. The next frontier uses powerful computational tools to unlock this data, transforming standard medical scans into rich sources of predictive information.
What is Radiomics?
Radiomics is a "digital biopsy" that analyzes medical images far beyond what is visually apparent. Specialized software extracts thousands of quantitative features from a scan, measuring subtle variations in texture, shape, and intensity. This process creates a unique data profile, or "radiomic signature," for the tumor. This signature can reflect underlying biological properties, potentially revealing a cancer's aggressiveness or genetic makeup without an invasive procedure.
The Role of Artificial Intelligence
The massive datasets generated by radiomics are too complex for human interpretation alone, which is where artificial intelligence (AI) and machine learning come in. Algorithms are trained on thousands of patient images linked to clinical outcomes. By analyzing these examples, the AI learns to identify subtle patterns in radiomic signatures that predict a tumor's behavior, such as its response to a specific therapy.
Potential Clinical Applications in Neuroblastoma
The combination of radiomics and AI holds immense promise for personalizing neuroblastoma care. For instance, an AI tool could analyze a child's initial scan and help predict whether the tumor is high-risk or low-risk, guiding treatment intensity from day one. It could also monitor therapy more effectively by detecting microscopic changes in tumor texture that signal a positive response, allowing for faster adjustments to a child’s treatment plan.