A corneal dystrophy is a condition where the cornea, the clear front part of the eye, loses its normal transparency due to a buildup of cloudy material. These conditions are often inherited and can affect different layers of the cornea, leading to a range of symptoms from mild discomfort to severe pain and vision loss. With more than 20 distinct types of corneal dystrophies, understanding the available treatments is crucial for managing symptoms and preserving sight. The approach to treatment is highly individualized, depending on the specific type of dystrophy, the severity of the condition, and how significantly it impacts a person's daily life and vision.
Treatment strategies vary widely, beginning with conservative measures and progressing to more advanced procedures as needed. For many individuals, initial management focuses on alleviating symptoms and correcting vision problems. For instance, in the early stages of Keratoconus, where the cornea thins and bulges into a cone shape, vision changes can often be corrected with eyeglasses. As the condition progresses, specialized contact lenses may be required to address worsening astigmatism. For other conditions like Fuchs' Dystrophy, which causes corneal swelling, doctors may prescribe saline eyedrops or ointments to draw fluid out of the cornea and reduce discomfort. In cases of Map-Dot-Fingerprint Dystrophy, where the outer layer of the cornea is prone to erosion, treatment is centered on pain management using lubricating eye drops, ointments, or even patching the eye to promote healing.
When a corneal dystrophy progresses to a point where vision is significantly harmed or conservative treatments are no longer effective, more advanced interventions may be recommended. Some of these treatments are designed to halt the progression of the disease or repair damage to the corneal surface.
- Corneal collagen crosslinking is a procedure that has been shown to stop the progression of Keratoconus, strengthening the cornea to prevent further bulging.
- Phototherapeutic keratectomy (PTK) is a laser treatment that can remove diseased layers or surface irregularities from the cornea. It is a valuable option for treating recurrent Lattice Dystrophy in a donor cornea or for addressing issues related to Map-Dot-Fingerprint Dystrophy.
- Other minor procedures, such as anterior corneal punctures or corneal scraping, can help treat the painful erosions associated with Map-Dot-Fingerprint Dystrophy by improving how cells adhere to the cornea or by removing damaged tissue to allow for healthy regrowth. In the most severe cases, where the cornea becomes heavily scarred or clouded, a corneal transplant may be necessary. This surgical procedure is a viable treatment for advanced Keratoconus, Fuchs’ Dystrophy, and Lattice Dystrophy, offering a chance to restore clarity and improve vision.
What is the most common cause of corneal disease?
The causes of corneal disease are incredibly varied, but several conditions stand out as particularly common. Minor injuries, such as corneal abrasions from scratches or foreign bodies, are frequent occurrences that affect the cornea's outermost layer. Infections, known as keratitis, also represent a significant and serious category of corneal problems, with improper contact lens hygiene being a leading and preventable cause. Additionally, conditions like dry eye, which becomes more prevalent with age, and environmental factors like sun and dust exposure can lead to chronic irritation and related corneal issues such as pterygium.
What are the symptoms of granular corneal dystrophy?
Patients with granular corneal dystrophy experience a range of symptoms as tiny, opaque deposits, often likened to breadcrumbs, accumulate on the cornea. A primary complaint is vision impairment, which can manifest as blurred or clouded vision, increased sensitivity to light (photophobia), and glare. Many individuals also report significant pain or discomfort, often described as a foreign body sensation, as if there are small pebbles in the eye. This pain is frequently linked to recurrent corneal erosions (RCE), a common complication where the outer layer of the cornea breaks down, which can also cause watery eyes. As the condition progresses, the deposits can grow and merge, further compromising vision.
Can corneal disease lead to blindness?
Yes, diseases affecting the cornea are a major cause of vision loss and can lead to irreversible blindness. The cornea must remain transparent to properly focus light into the eye, but various conditions can cause it to become scarred or clouded, a process known as corneal opacification. This damage blocks light from reaching the retina, impairing vision. Globally, corneal blindness is the fourth leading cause of blindness, with major causes including infections like bacterial and fungal keratitis, trachoma, and progressive thinning disorders such as keratoconus. Ocular trauma, ulcerations, and certain autoimmune diseases also contribute significantly, making corneal disease a leading cause of preventable blindness worldwide, affecting millions of individuals.
What is the most common treatment for corneal damage?
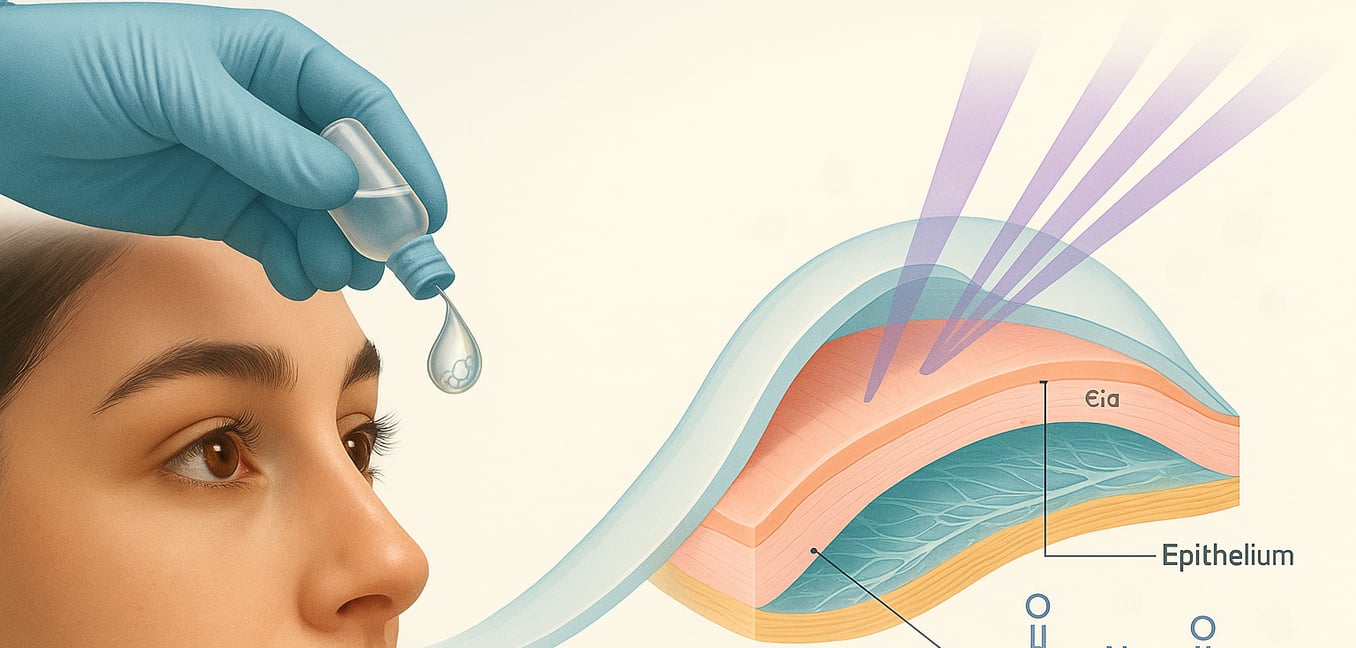
For common superficial damage, such as a corneal abrasion, the treatment is typically straightforward, as these injuries often heal within 2 to 3 days. The mainstay of therapy involves prescribing topical antibiotic eye drops or an ointment to lubricate the eye and prevent infection while the cornea's surface layer, the epithelium, regenerates. To manage the significant discomfort and light sensitivity that can accompany these injuries, doctors often recommend oral pain relievers like nonsteroidal anti-inflammatory drugs (NSAIDs) or prescribe specific topical ophthalmic drops. In addition to these medications, patients are advised to stop wearing contact lenses and, in some cases, may use a temporary bandage contact lens to protect the eye and aid healing.
Can corneal dystrophy reversed?
While there is currently no definitive "cure" that permanently reverses the underlying genetic cause of most corneal dystrophies, the symptoms and pathological changes can often be effectively reversed through various treatments. For instance, procedures like superficial keratectomy can remove abnormal tissue buildup in conditions such as Anterior Basement Membrane Dystrophy, allowing for the regrowth of a healthier, more stable corneal surface. Similarly, in advanced cases of Fuchs' dystrophy, corneal transplant surgeries like Descemet membrane endothelial keratoplasty (DMEK) replace the diseased endothelial cell layer with healthy donor tissue, restoring corneal clarity and reversing vision loss for many years. Looking ahead, emerging gene therapy approaches are being investigated with the goal of directly correcting the genetic mutations responsible for these conditions, which could offer a more fundamental and lasting reversal of the disease process in the future.
What eye drops are good for corneal scarring?
Topical losartan eye drops are an emerging and effective off-label treatment for vision-impairing corneal scarring. This medication works by disrupting the TGF-beta signaling pathway, which prevents the development of scar-forming myofibroblasts and encourages the resolution of existing fibrosis. While not yet commercially mass-produced, losartan drops can be prepared by compounding pharmacies, with a concentration of 0.8 mg/mL administered six times daily being a commonly used and safe dosage. In cases where scarring is caused by inflammation, such as after LASIK, corticosteroids are used to treat the inflammation itself, and losartan may be added to minimize the resulting scar tissue. Treatment is often long-term, requiring several months of consistent use for the fibrosis to resolve and for the corneal basement membrane to regenerate.
Is fuchs dystrophy an autoimmune disease?
Fuchs endothelial corneal dystrophy (FECD) is not considered a classic autoimmune disease; it is primarily categorized as a genetic and degenerative condition driven by oxidative stress and abnormal protein deposition. While FECD is described as a "primarily non-inflammatory disorder," emerging evidence suggests that inflammation and a disruption of the eye's immune privilege contribute to its progression. Studies have detected elevated levels of inflammatory chemokines, such as RANTES, eotaxin, and IP-10, in the aqueous humor of patients with FECD. This indicates that while the disease may not be initiated by an autoimmune attack, a local inflammatory response is present and likely contributes to the cycle of corneal endothelial cell damage.