Understanding Congenital Toxoplasmosis
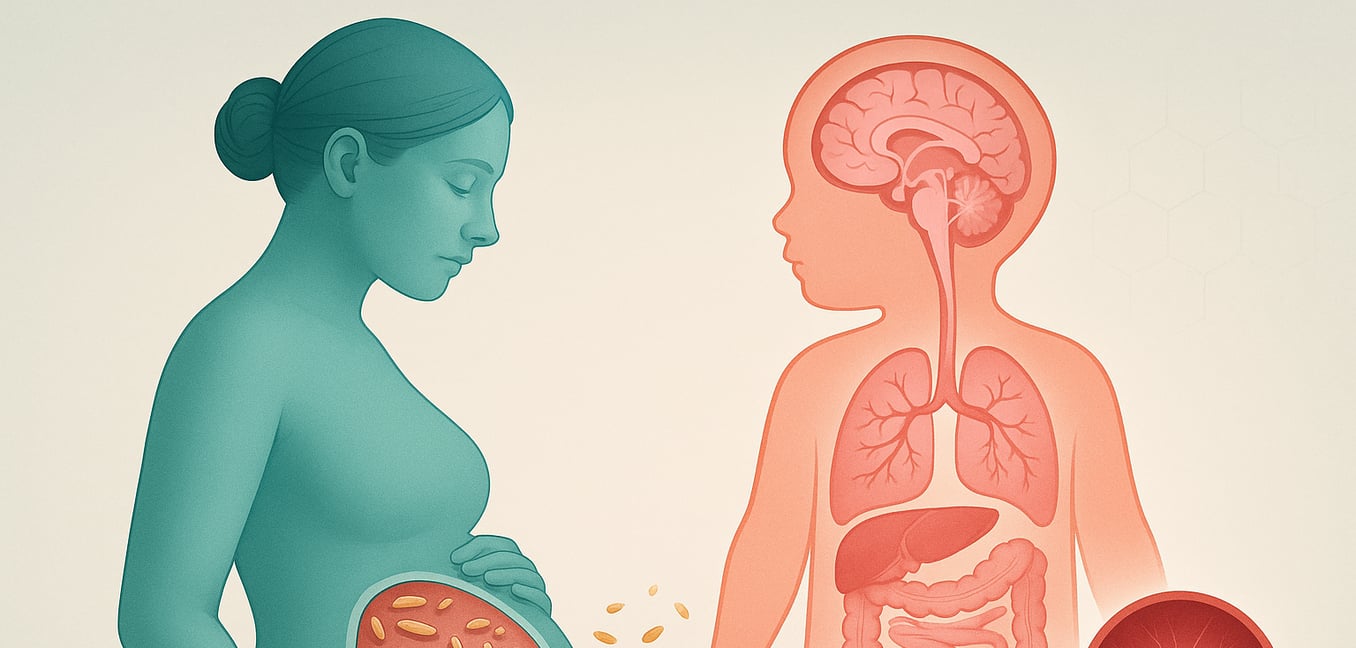
Congenital toxoplasmosis is an infection that occurs when the Toxoplasma gondii parasite is transmitted from a mother to her unborn child during pregnancy. While an infected mother often experiences only mild, flu-like symptoms or none at all, the consequences for a developing fetus can be severe. The parasite's ability to cross the placenta makes it a significant concern in prenatal care, as the timing of the infection dramatically influences the outcome.
The risk and severity are a paradox of pregnancy. An infection in the first trimester is less likely to be transmitted to the fetus, but if it is, the damage is often catastrophic because fundamental organ systems are just beginning to form. Conversely, a third-trimester infection has a much higher chance of reaching the baby, but the health problems are typically less severe, as major development is already complete.
How the Parasite Disrupts Fetal Development
Once the parasite crosses the placental barrier, it can directly interfere with the fundamental processes that build the body’s most critical structures, particularly the brain and muscles. This disruption happens at a cellular level, leading to severe and permanent damage before birth.
In the developing brain, the infection triggers a destructive process. Rather than forming a dense, organized network, the brain tissue of an affected fetus can show reduced cell density and signs of widespread cell death. This damage can happen even in areas where the parasite isn't physically present, as proteins it releases can cause inflammation and trigger brain cells to self-destruct. This cellular-level sabotage is a direct cause of visible malformations like microcephaly, an abnormally small head.
Muscle formation is also severely hampered. In a healthy fetus, immature muscle cells fuse to create long, strong muscle fibers. The infection disrupts this crucial fusion process, leaving muscle tissue with fewer and weaker fibers. Instead, the tissue becomes filled with disorganized cells that failed to properly merge. This stalled development can lead to malformed limbs or even the absence of entire muscle groups. A key mechanism behind this damage is the parasite's ability to break down the molecular "glue" that holds cells together, preventing them from forming stable, functional tissue in both the brain and muscles.
The Lifelong Impact: From Birth Defects to Delayed Threats
The developmental damage caused by congenital toxoplasmosis results in a wide spectrum of outcomes, ranging from immediately apparent birth defects to hidden threats that emerge years later. The most severe cases can result in miscarriage, stillbirth, or profound disabilities visible at birth, such as seizures or significant physical malformations.
However, one of the most insidious aspects of the disease is that the vast majority of infected newborns—around 85%—appear perfectly healthy. This asymptomatic presentation masks an underlying infection, as the parasite can lie dormant in the body for years before reactivating.
The most common delayed consequence is damage to the eyes. Inflammation of the retina, known as chorioretinitis, can flare up unpredictably during childhood or adolescence, causing blurred vision, pain, and light sensitivity. Each flare-up, caused by the reactivation of dormant parasite cysts, can create new scars on the retina. If these scars affect central vision, they can lead to progressive and permanent visual impairment.
Subtle neurological and developmental challenges can also surface as a child grows. An infant who was asymptomatic at birth may later struggle with learning disabilities, poor coordination, or mild cognitive deficits that only become apparent in a school setting. These issues may stem from tiny, undetected areas of damage in the brain from the initial infection. Similarly, hearing impairment is another serious delayed outcome. The parasite can damage the auditory system, leading to hearing loss that develops so gradually it may be missed or misattributed to other issues.
A Potential Link to Autism Spectrum Disorder
Emerging research is exploring a potential, though not yet proven, link between maternal Toxoplasma infection and the risk of autism spectrum disorder (ASD) in offspring. Scientists have noted intriguing parallels in the brain changes and immune responses seen in both conditions, prompting investigation into several possible connections.
One area of focus is the mother's immune response during pregnancy. Studies have found correlations between a mother's antibody levels to Toxoplasma and the likelihood of her child developing autism, suggesting the specific timing and nature of her immune reaction may influence fetal brain development.
The parasite may also directly interfere with the brain's chemical balance. Research has shown that Toxoplasma gondii can alter levels of dopamine, a critical neurotransmitter involved in mood, motivation, and motor control. Since dysregulated dopamine signaling is also a feature of ASD, this presents a plausible biochemical pathway through which the infection could contribute to the condition.
Perhaps the most compelling evidence involves mitochondria, the energy-producing powerhouses of our cells. Autism is increasingly linked to mitochondrial problems, and recent studies have found mutations in the mitochondrial DNA of autistic children who also had congenital toxoplasmosis. The theory is that the parasite, which relies on the host cell's energy to multiply, may damage these energy pathways, leading to stress and impairing the healthy development of the nervous system.
Preventing Developmental Injuries Through Prenatal Screening
Given the severe and often hidden consequences of congenital toxoplasmosis, a proactive approach centered on prenatal screening is the most effective tool for protecting unborn children. National programs in countries like France and Austria have proven that a systematic strategy of testing and treatment can dramatically reduce both the rate and severity of the infection. This preventative framework is built on several key actions.
-
Early Detection: Regular blood tests for expectant mothers can identify a new infection as soon as it occurs, allowing for immediate treatment to block the parasite from being transmitted to the fetus.
-
In-Utero Treatment: If transmission has already happened, medications given to the mother can cross the placenta to fight the infection in the fetus, minimizing damage to the developing brain and eyes and reducing the severity of the disease at birth.
-
Post-Birth Care: Screening ensures that infected newborns, even those without symptoms, receive a year-long course of treatment. This therapy attacks any remaining dormant parasites, significantly lowering the risk of delayed consequences like vision or hearing loss later in life.
-
Cost-Effectiveness: The cost of a national screening program is minimal compared to the enormous lifetime expense of medical care and support for a child with severe disabilities. Preventing just a few severe cases can offset the entire annual cost of a program, making it a sound public health investment.