Understanding ALAD Deficiency Porphyria (ADP)
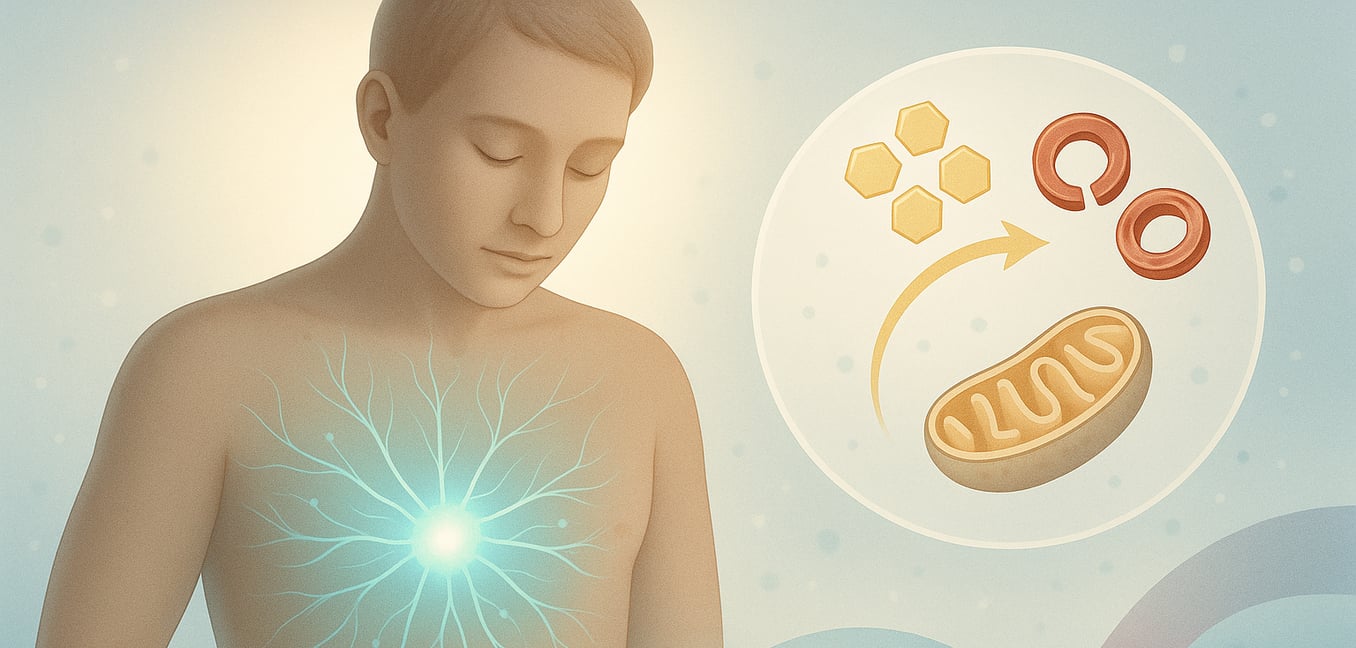
ALAD Deficiency Porphyria, or ADP, is an extremely rare genetic disorder. It affects the body's ability to produce heme, an essential molecule involved in many vital processes, including carrying oxygen in the blood. The problem lies with an enzyme called delta-ALA dehydratase (ALAD), which is a key worker in the heme production pathway.
In ADP, the ALAD enzyme doesn't function correctly due to inheriting a faulty gene from both parents (an autosomal recessive inheritance pattern). When ALAD is deficient, a substance called aminolevulinic acid (ALA) builds up in the body. This accumulation of ALA is primarily responsible for the symptoms of ADP. Unlike some other related conditions called acute porphyrias, the level of another substance, porphobilinogen (PBG), in the urine usually remains normal in ADP. This can be an important clue for doctors.
Diagnosing ADP involves specific blood tests that measure the activity of the ALAD enzyme. Since other conditions, like lead poisoning or certain hereditary disorders, can also affect ALAD activity, doctors must carefully rule these out through a thorough medical history and additional tests before confirming ADP.
The Core Crisis: Acute Attacks
ADP typically manifests as sudden, severe episodes known as acute attacks. These attacks can be debilitating and often require hospital care.
Severe Abdominal Pain: The Leading Symptom
The most common and often the first indicator of an ADP attack is intense abdominal pain. This isn't a minor ache; it's typically described as severe, widespread, and often crampy or colicky. A peculiar feature of this pain is that it originates from nerve dysfunction (neuropathic pain) rather than inflammation of abdominal organs. Consequently, a physical examination of the abdomen might reveal surprisingly little tenderness, despite the patient reporting extreme pain. This discrepancy can be a puzzle for doctors unfamiliar with porphyria and may lead to delays in diagnosis or unnecessary investigations for other abdominal conditions like appendicitis or gallbladder problems.
Accompanying Gastrointestinal Distress
The severe abdominal pain in ADP is rarely an isolated symptom. It is frequently accompanied by other distressing gastrointestinal issues:
- Nausea and Vomiting: Significant nausea and repeated vomiting are very common. These can make it hard for individuals to eat or drink, potentially leading to dehydration and electrolyte imbalances, which can worsen the overall condition. Strong anti-nausea medications are often needed.
- Constipation: This is another frequent complaint, adding to abdominal discomfort and bloating.
- Ileus: In severe cases, the bowel may temporarily lose its ability to contract and move contents along, a serious condition called ileus, which requires careful medical management.
- Diarrhea: Though less common than constipation, diarrhea can occasionally occur.
The intensity of the abdominal pain usually requires strong pain-relieving medications, such as opioids, administered in a hospital setting. Effective pain control is crucial, as uncontrolled pain can increase stress and potentially worsen the attack.
Widespread Neurological Impact
Beyond the abdomen, ADP attacks can profoundly affect the nervous system, leading to a range of neurological symptoms. These can involve peripheral nerves, the central nervous system (brain and spinal cord), and the autonomic nervous system (which controls involuntary body functions).
Peripheral Neuropathy: Sensory and Motor Disturbances
Damage to peripheral nerves (nerves outside the brain and spinal cord) is a common feature of ADP attacks. This can cause:
- Sensory symptoms: These may begin as pain in the back, arms, or legs, tingling sensations, or numbness.
- Motor symptoms: Muscle weakness (paresis) is a significant concern. It can start in the limbs and may progress. In severe cases, the weakness can affect the muscles responsible for breathing, leading to respiratory difficulties—a life-threatening emergency that may require mechanical ventilation.
Central Nervous System (CNS) Effects
The brain and spinal cord can also be affected during an ADP attack:
- Seizures: These are a serious risk. Managing seizures in ADP can be challenging because many standard anti-seizure medications are unsafe for people with porphyria as they can trigger or worsen attacks.
-
Psychiatric and Cognitive Changes:
A wide array of neuropsychiatric symptoms can occur. These may include:
- Anxiety, restlessness, or agitation
- Insomnia (difficulty sleeping)
- Confusion, disorientation, or delirium (an altered state of awareness)
- Hallucinations (seeing or hearing things that aren't there)
- Mood disturbances, such as depression or symptoms resembling bipolar disorder
- In rare, severe cases, psychosis or catatonia.
Autonomic Nervous System Dysfunction
The autonomic nervous system, which regulates functions like heart rate, blood pressure, and digestion, is often disrupted in ADP. This dysfunction contributes to many symptoms experienced during an attack:
- Cardiovascular Signs: A rapid heart rate (tachycardia) and high blood pressure (hypertension) are frequently observed and can be quite pronounced. These signs indicate significant physiological stress and may require medication to manage. Less commonly, other heart rhythm problems (arrhythmias) can occur.
- Other Autonomic Symptoms: Excessive sweating, dizziness upon standing (postural hypotension), and bladder problems (such as difficulty urinating, sometimes requiring a catheter) can also result from autonomic nervous system involvement.
Other Important Systemic Effects
ADP attacks can lead to disturbances in other body systems, further complicating the clinical picture.
Endocrine Imbalances: The Risk of Hyponatremia
A critical concern during ADP attacks is the development of low sodium levels in the blood, a condition called hyponatremia. This often occurs due to the Syndrome of Inappropriate Antidiuretic Hormone secretion (SIADH), where the body produces too much of a hormone that causes it to retain water, diluting sodium levels. Hyponatremia is particularly dangerous because it can worsen neurological symptoms, such as confusion and seizures, and in severe instances, can lead to coma. Careful monitoring and correction of sodium levels are vital.
Potential for Kidney Complications
While information specific to long-term kidney health in the few documented ADP cases is limited due to the disorder's extreme rarity, kidney problems are a known concern in other acute porphyrias that share similar attack mechanisms. Recurrent acute attacks and the persistent high blood pressure often seen during these episodes can put a strain on the kidneys over time. This can potentially contribute to the development of chronic kidney disease. Prompt and effective management of acute attacks is therefore important for protecting overall kidney health.
Understanding Attack Triggers
Symptoms of ADP manifest as acute attacks, which can be precipitated by various factors. These triggers often increase the body's demand for heme production, overwhelming the already deficient ALAD enzyme and leading to the accumulation of ALA. Common triggers include:
- Certain medications (e.g., barbiturates, sulfa antibiotics, some hormonal drugs)
- Hormonal fluctuations (e.g., related to the menstrual cycle)
- Significant dietary changes, especially fasting or very low-carbohydrate diets
- Alcohol consumption
- Infections
- Surgical procedures
- Periods of intense emotional or physical stress
Identifying and avoiding known triggers is an important part of managing ADP, although some attacks may occur without an obvious cause.