Types of Corneal Transplants for Corneal Dystrophy
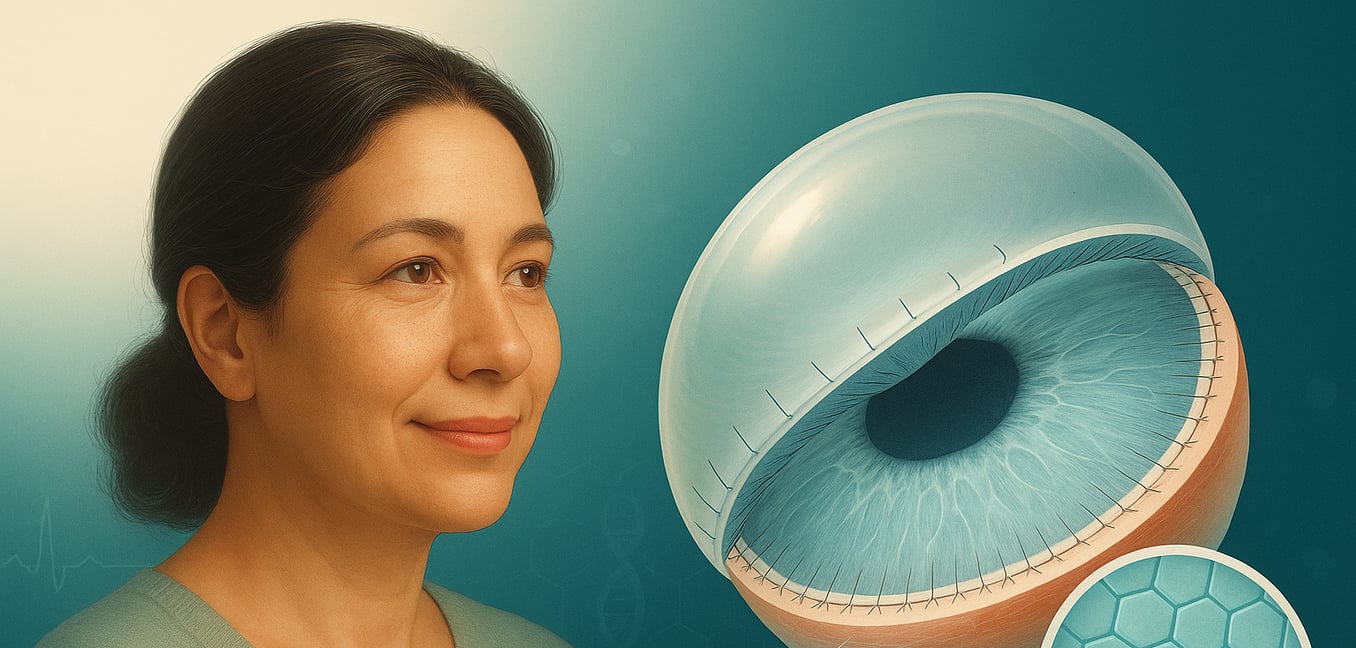
Your cornea is the clear, dome-shaped window at the front of your eye, essential for focusing light and providing clear vision. Corneal dystrophies are a group of genetic conditions that cause abnormal material to build up in the cornea, making it cloudy and impairing sight over time.
When vision loss becomes significant and can no longer be corrected with glasses or contacts, a corneal transplant, also known as keratoplasty, becomes the most effective treatment. The goal is to replace the diseased corneal tissue with healthy tissue from a donor.
Modern surgery offers several types of transplants. Rather than replacing the entire cornea every time, surgeons can now selectively replace only the specific layers affected by the dystrophy. This targeted approach leads to faster recovery and better outcomes. Here are the main types of corneal transplants available today.
The Traditional Approach: Full-Thickness Penetrating Keratoplasty (PKP)
For over a century, penetrating keratoplasty (PKP) has been the standard for corneal transplantation. This full-thickness procedure replaces all layers of the central cornea with healthy donor tissue, making it a comprehensive solution when the entire cornea is damaged.
When is PKP Recommended?
PKP is the preferred option when a corneal dystrophy or injury affects all layers of the cornea. This includes conditions like advanced keratoconus, where the cornea is severely misshapen, or in cases of deep, full-thickness scarring from past trauma or infections. It provides a complete structural and optical reset for the eye.
The Surgical Procedure
During PKP, a surgeon uses a circular instrument called a trephine to remove the damaged central disc of the cornea. A precisely matched "button" of healthy donor cornea is then carefully stitched into place with numerous ultra-fine sutures that hold the new tissue securely as it heals.
Recovery and Considerations
Visual recovery after PKP is a gradual process, often taking a year or more to fully stabilize. Because the entire cornea is replaced and held with many sutures, there are specific risks to consider:
- High Astigmatism: Suture tension can warp the new cornea's shape, distorting vision. This often requires correction with special rigid contact lenses or additional surgery.
- Higher Rejection Risk: Because the entire donor tissue is foreign to the body, the immune system is more likely to attack it.
- Long-Term Medication: Patients typically need to use anti-rejection steroid eye drops for many years, sometimes for life, to protect the graft.
Preserving the Innermost Layer: Deep Anterior Lamellar Keratoplasty (DALK)
Deep Anterior Lamellar Keratoplasty (DALK) is a sophisticated partial-thickness transplant that replaces the front and middle layers of the cornea while preserving your own healthy inner layer (the endothelium). It is an ideal treatment for conditions that affect the cornea's main structural layer, the stroma, but leave the endothelium unharmed.
Who is a Good Candidate?
DALK is an excellent choice for treating keratoconus, a condition where the stroma thins and bulges outward into a cone shape. It is also used for deep scars or cloudiness in the cornea's front layers that do not affect the endothelium.
Key Advantages
The greatest benefit of DALK is a dramatically lower risk of graft rejection. Your endothelium is the layer most often targeted by the immune system, so keeping your own means the graft is much more likely to remain clear for decades. This also reduces the need for long-term steroid eye drops. Furthermore, because the eye is not fully opened during surgery, it remains structurally stronger and more resistant to injury after healing.
Targeting the Inner Cornea: Descemet Stripping Endothelial Keratoplasty (DSEK/DSAEK)
When a corneal dystrophy like Fuchs’ primarily damages the innermost layer of the cornea, a highly specialized transplant called DSEK (or DSAEK) is performed. This technique replaces only the thin, diseased back layer of the cornea, leaving the healthy front layers of your eye completely untouched.
How the Procedure Works
Instead of a large circular incision, the surgeon makes a small opening on the side of the eye. A thin, folded layer of donor tissue is inserted and unfolded inside the eye. To hold this new layer in place, the surgeon injects an air bubble that presses the graft against the back of your cornea until it adheres on its own, eliminating the need for sutures.
Faster Recovery and Better Vision
Because the front surface of the cornea remains smooth and unchanged, vision improves much more quickly than with PKP. Many patients notice a significant improvement within a few weeks to a couple of months. The final vision is often sharper because the procedure induces very little astigmatism.
A Unique Post-Operative Requirement
The success of the surgery depends on the air bubble holding the graft in place. For the first 24 to 48 hours, patients are instructed to lie flat on their back as much as possible, looking up at the ceiling. This ensures the bubble remains in the correct position for the graft to attach successfully.
The Ultra-Thin Graft: Descemet Membrane Endothelial Keratoplasty (DMEK)
DMEK is the most refined and advanced form of partial-thickness corneal transplantation. This procedure replaces only the Descemet membrane and its single layer of endothelial cells—a donor graft that is just one-hundredth of a millimeter thick. It offers the potential for the clearest vision possible.
The Potential for Superior Vision
The DMEK graft is incredibly delicate and contains no extra tissue, allowing for a perfect anatomical and optical fit. This precision often results in superior visual outcomes, with a higher likelihood of achieving 20/25 or even 20/20 vision. By transplanting the absolute minimum amount of foreign tissue, DMEK also has the lowest risk of graft rejection.
Surgical Delicacy and Considerations
The extreme thinness of the DMEK graft makes it very challenging for the surgeon to handle. It behaves like a transparent scroll inside the eye and must be carefully uncurled and positioned. Because of this complexity, there is a slightly higher chance the graft may not fully attach, sometimes requiring a second, minor procedure to inject another air bubble (a "rebubble") to press it back into place.