Fuchs endothelial corneal dystrophy (FECD) is a common, progressive disease affecting the innermost layer of the cornea, the clear front part of the eye. This layer is lined with endothelial cells, which act like tiny pumps to maintain the cornea's fluid balance and transparency. In FECD, these cells gradually die off, causing fluid to accumulate, which leads to corneal swelling (edema), blurred vision, glare, and halos. While the definitive treatment has traditionally been corneal transplantation, significant advancements are offering new hope through less invasive and more targeted therapies that aim to preserve or restore vision with fewer complications and faster recovery times.
The field of corneal transplantation has evolved from replacing the entire cornea to more refined partial-thickness procedures like Descemet’s membrane endothelial keratoplasty (DMEK), where only the diseased inner layer is replaced. Recent research focuses on improving the DMEK procedure itself, particularly in how the delicate donor tissue—which is as thin as plastic wrap—is prepared and handled. For instance, a study comparing the traditional "modified Jones tube" with a newer tool called the DMEK EndoGlide found that the new device provides surgeons with better control, leading to a faster and smoother implantation process. This refinement is crucial as it helps preserve more of the vital endothelial cells, potentially improving long-term graft survival and visual outcomes. Other surgical trials are exploring technologies like intraoperative optical coherence tomography (OCT) to give surgeons real-time, high-resolution images during surgery for more precise graft placement.
Beyond refining surgery, a major frontier in treating FECD involves non-surgical and regenerative approaches that could delay or even eliminate the need for a transplant. These emerging therapies fall into several categories:
- Pharmacological treatments: Eye drops containing Rho-associated kinase (ROCK) inhibitors, such as netarsudil, are showing promise in clinical trials. These medications can help the remaining endothelial cells to spread out, adhere, and regenerate, thereby reducing corneal swelling and improving vision. Other drugs being investigated include mitochondrial protectors and growth factors that aim to halt cell death and encourage healing.
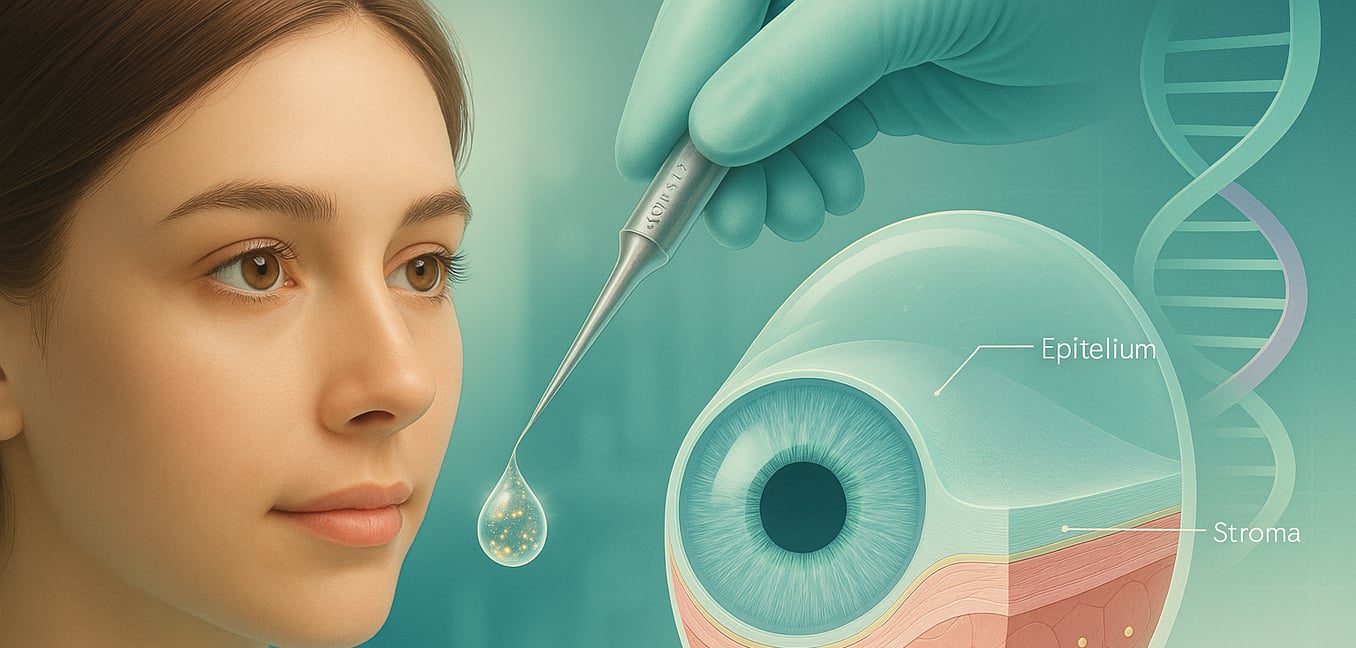
- Cell-based therapy: This cutting-edge approach involves injecting lab-grown human corneal endothelial cells directly into the eye. A key innovation is the use of magnetic nanoparticles to tag these cells, allowing a magnet to guide them to the correct location on the inner cornea to form a new, healthy layer. This could one day offer a minimally invasive alternative to transplantation, bypassing the need for donor tissue entirely.
- Gene therapy: Since many cases of FECD are linked to a specific genetic mutation, researchers are developing therapies that target the root cause. One such treatment is designed to correct the faulty genetic messaging that leads to endothelial cell death. While still in early stages, gene therapy holds the potential to provide a permanent, personalized cure for patients with this genetic form of the disease.
Can you have cataract surgery if you have corneal dystrophy?
Yes, you can have cataract surgery if you have a corneal dystrophy like Fuchs' dystrophy, as it is a common situation for surgeons to manage. The surgical plan is personalized based on the severity of your corneal condition. If the dystrophy is mild, cataract surgery alone can often be performed successfully using special techniques and protective agents to minimize stress on the cornea's delicate inner layer. For more advanced cases with significant corneal swelling or a low endothelial cell count, your ophthalmologist may recommend a combined procedure. This single operation removes the cataract and simultaneously replaces the diseased inner layer of your cornea with healthy donor tissue (a procedure called endothelial keratoplasty) to achieve the best long-term visual outcome.
Can you drive with Fuchs corneal dystrophy?
While many individuals with Fuchs’ endothelial corneal dystrophy (FECD) maintain normal vision on standard eye charts, their ability to drive safely can be significantly compromised, especially at night. A study using an advanced driving simulator revealed that patients with FECD experienced major impairments when driving in simulations with glare from oncoming headlights. Even with 20/20 vision, these patients recognized 14% fewer roadside hazards and needed to be almost twice as close to a hazard to identify it compared to individuals without the disease. This difficulty is linked to subclinical corneal changes that standard vision tests may not capture, creating a critical discrepancy between a person's tested visual acuity and their real-world functional ability to drive safely.
Can you reverse corneal thinning?
While treatments for corneal thinning conditions like keratoconus are typically designed to slow or stop the disease's progression, some clinical evidence suggests a reversal of thinning may be possible in certain cases. The primary procedure used to strengthen the cornea, corneal collagen cross-linking (CXL), has been shown to halt further thinning. Remarkably, in at least one documented case of a patient with Terrien marginal degeneration (TMD), CXL treatment led to a measurable increase in corneal thickness in the thinned areas of both eyes over several years. Researchers speculate this reversal occurs because CXL increases the cornea's resistance to enzymatic breakdown, which may shift the natural balance toward collagen synthesis and tissue rebuilding.
Who treats corneal dystrophy?
Treatment for corneal dystrophy is managed by eye care professionals. Your journey may begin with an optometrist, who can perform initial diagnostic tests, such as a cornea examination, and prescribe nonsurgical treatments like saline eye drops or soft contact lenses for pain relief. For more advanced cases or specialized care, you will be referred to an ophthalmologist, a medical doctor specializing in eye surgery and disease. These specialists, particularly those with expertise in corneal conditions, can determine if you are a candidate for surgical procedures. They are qualified to perform complex surgeries such as Descemet membrane endothelial keratoplasty (DMEK) or a full-thickness cornea transplant to restore vision when the disease progresses.
What is the most common treatment of corneal damage?
The most common treatment for a corneal abrasion focuses on preventing infection and managing discomfort while the eye heals, a process that usually takes a few days for minor injuries. Doctors typically prescribe prophylactic topical antibiotic eye drops or ointments to prevent bacterial complications, with specific antibiotics chosen for contact lens wearers to cover for more aggressive organisms. Pain and inflammation are managed with oral nonsteroidal anti-inflammatory drugs (NSAIDs) or specialized topical NSAID eye drops. For more severe pain and light sensitivity, a doctor may also use a short-acting cycloplegic drop to relax the eye's focusing muscles or place a soft, bandage-like contact lens over the cornea to act as a protective shield and promote comfortable healing.
How can I improve my corneal dystrophy?
You can improve your corneal dystrophy through various treatments tailored to your specific condition and symptoms. For early or mild cases, supportive measures like saline eye drops to reduce corneal swelling, lubricating drops for comfort, and specialized contact lenses can improve vision and relieve pain. If your vision becomes significantly limited, your ophthalmologist may recommend a procedure such as phototherapeutic keratectomy (PTK) to smooth the corneal surface or a lamellar keratectomy to remove superficial opacities. In more advanced cases, a corneal transplant—either replacing partial layers (lamellar keratoplasty) or the full thickness of the cornea—may be required to restore clear vision by using healthy donor tissue.
What foods are good for Fuchs dystrophy?
While no specific diet can cure Fuchs dystrophy, certain nutritional choices may help manage symptoms and support overall corneal health. A diet rich in antioxidants, found in foods like fruits and vegetables, is recommended to help combat the oxidative stress that contributes to endothelial cell damage. Reducing sodium intake is also crucial, as a low-sodium diet can help regulate corneal hydration levels and potentially lessen the morning blurriness associated with corneal edema. Additionally, staying well-hydrated and managing systemic conditions like diabetes and hypertension through a healthy diet can further support the health of your corneas by preventing accelerated endothelial cell loss.