An Introduction to Marfan Syndrome
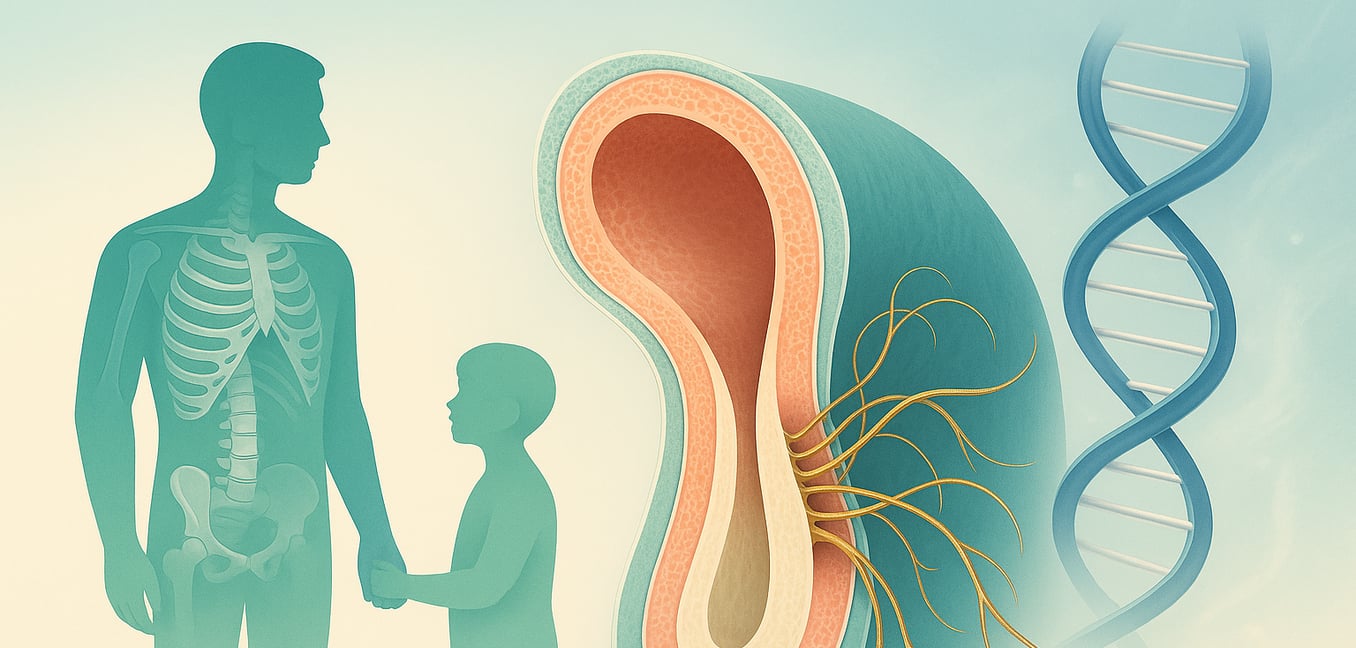
Marfan syndrome is a genetic disorder that affects the body’s connective tissue, the essential material that acts as a glue and scaffold for organs, blood vessels, bones, and muscles. Since connective tissue is present throughout the body, the condition can lead to a wide and varied range of health challenges, most notably affecting the skeleton, heart, and eyes.
Individuals with the syndrome are often unusually tall and slender, with long limbs and digits. They may also develop a curved spine, known as scoliosis, or a chest that sinks inward or protrudes. However, the most life-threatening complications involve the cardiovascular system, particularly the aorta—the body's main artery. Weakened tissue can cause the aorta to stretch and enlarge, creating a high risk of a sudden, dangerous tear. The syndrome's impact is highly variable; even within the same family, some individuals may have only mild physical traits while others face severe, progressive complications, underscoring the need for careful medical management.
The FBN1[^2] Gene: From Blueprint to Malfunction
At the heart of Marfan syndrome is a mutation in a single gene: FBN1. Located on chromosome 15, this gene contains the instructions for making fibrillin-1, a large protein that is a critical building block for the body's connective tissue. Fibrillin-1 proteins assemble into thread-like structures called microfibrils, which form a supportive mesh around cells. These microfibrils give tissues like the aorta their elasticity and provide structural support to more rigid parts of the body, like bones and the ligaments holding the eye’s lens in place. A faulty FBN1 gene disrupts this entire process, leading to the systemic weakness seen in Marfan syndrome.
How Mutations Disrupt Fibrillin-1
A change in the FBN1 gene can compromise connective tissue in two primary ways:
-
Producing too little protein (Haploinsufficiency). Some mutations result in the body producing an insufficient amount of functional fibrillin-1. In this scenario, one of the two FBN1 gene copies is non-working, so the body can only rely on the single healthy copy. This isn't enough to meet the body’s needs. Think of it as trying to build a brick wall with only half the required bricks—the resulting structure is inherently weak and incomplete.
-
Producing a faulty, interfering protein (Dominant-Negative Effect). Other mutations cause the gene to produce an altered, misshapen fibrillin-1 protein that actively sabotages the normal protein. This faulty protein gets incorporated into the microfibril structure alongside the healthy protein. This is like mixing crumbling, poorly made bricks in with the good ones; the defective components compromise the integrity of the entire wall, often leading to more severe structural problems.
The Downstream Effects on the Body
The breakdown in microfibril formation has consequences that extend beyond simple structural weakness. These supportive fibers have a crucial secondary job: they act as storage units for growth-regulating proteins, most notably Transforming Growth Factor-beta (TGF-β). Microfibrils normally keep TGF-β sequestered and inactive until it is needed for processes like tissue repair and development.
When FBN1 mutations cause microfibrils to become disorganized and fragmented, they can no longer hold onto TGF-β effectively. This leads to an excessive amount of active TGF-β being released into the tissues. This overactivity is believed to be a key driver of some of Marfan syndrome's most recognizable features, including the overgrowth of the long bones that results in a tall, thin build.
Inheritance Patterns: How Marfan Syndrome is Passed Down
Marfan syndrome follows an autosomal dominant inheritance pattern, which explains why it can affect multiple generations of a family but also appear unexpectedly in an individual with no family history. Understanding this pattern is key to genetic counseling and family planning.
- One faulty gene is enough. The term "autosomal dominant" means the FBN1 gene is on a non-sex chromosome (autosomal) and only one mutated copy from a parent is needed to cause the disorder (dominant). It affects males and females equally.
- A 50% chance with each pregnancy. A parent with Marfan syndrome has a 50/50 chance of passing the mutated gene to each of their children. This probability is independent for each child, like a coin toss.
- New mutations are common. In about 25% of cases, the condition arises from a new, or "de novo," mutation that occurs spontaneously in the egg or sperm cell. In these instances, the parents are unaffected, but the child will have Marfan syndrome and can pass it on to their own children.
- Severity is not inherited. Inheriting the FBN1 mutation does not predict how severe the symptoms will be. A parent with mild features can have a child with major complications, and vice versa. This variability makes individualized medical monitoring essential for everyone with the condition.
The Role of Genetic Testing in Diagnosis
Because the features of Marfan syndrome can vary so dramatically and overlap with other connective tissue disorders, genetic testing has become an essential tool for providing clear and accurate diagnoses. It allows doctors to look directly at the underlying genetic cause rather than relying on physical symptoms alone.
- Confirming the diagnosis. When clinical signs are ambiguous, finding a known disease-causing mutation in the FBN1 gene can provide a definitive diagnosis, ending uncertainty for patients and enabling doctors to create a proactive management plan.
- Distinguishing from similar disorders. Conditions like Loeys-Dietz syndrome can mimic Marfan syndrome but are caused by different gene mutations and often require more aggressive treatment, particularly for the aorta. Genetic panels that test for FBN1 and other related genes ensure the correct diagnosis is made.
- Enabling predictive testing for family members. Once a specific mutation is identified in a family, other at-risk relatives can be tested for that exact change. This can identify individuals who have the condition before symptoms appear, allowing for early, life-saving monitoring and treatment. It also relieves relatives who test negative from a lifetime of unnecessary screening.