Living with Omphalocele: A Guide for Families
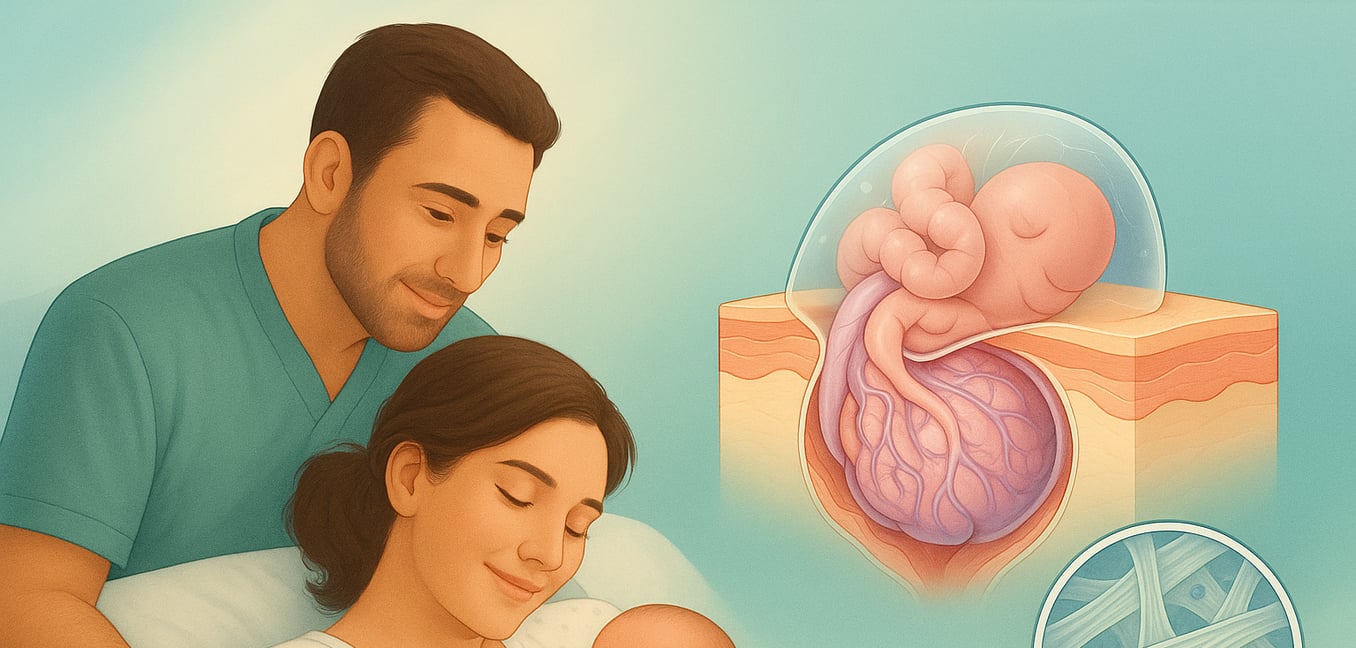
An omphalocele is a birth defect of the abdominal wall where a baby's intestines, liver, or other organs protrude through an opening at the base of the umbilical cord. These organs are covered by a thin, protective sac. This condition develops very early in pregnancy and is not caused by anything a parent did or did not do.
During early pregnancy, a baby's intestines grow so fast they temporarily bulge into the umbilical cord. This is a normal and expected stage of development. Around the twelfth week, as the baby's belly grows larger, these organs are supposed to return to the abdomen, and the abdominal wall closes. Omphalocele occurs when this final step is disrupted, and the organs remain outside in their protective sac. While the exact cause is often unknown, it is sometimes associated with certain genetic conditions.
Diagnosis and Preparing for Your Baby
A diagnosis is usually made during routine prenatal screenings, giving families and their medical team time to prepare. Once an omphalocele is identified, further tests are recommended to understand your baby's specific needs.
Prenatal Ultrasound
An ultrasound is the most common tool for identifying an omphalocele after 12 weeks of pregnancy. It shows the organs protruding at the base of the umbilical cord. Follow-up ultrasounds will be used to monitor the omphalocele's size, check which organs are involved, and track your baby’s overall growth to help plan for a safe delivery.
Fetal Echocardiogram
Because up to half of babies with an omphalocele also have a heart defect, your doctor will recommend a specialized ultrasound of your baby’s heart. This fetal echocardiogram allows a pediatric cardiologist to examine the heart's structure and function before birth, ensuring the medical team is prepared for any cardiac support needed after delivery.
Genetic Counseling and Testing
Omphalocele can be associated with chromosomal conditions. Your care team will likely discuss genetic testing, such as amniocentesis, which tests a small sample of amniotic fluid. This information helps create the most appropriate care plan for your baby.
Comprehensive Evaluation
Your medical team will conduct a thorough evaluation, as babies with omphalocele can sometimes have other health challenges affecting the lungs, digestion, or skeletal system. Identifying these early helps create a complete picture of your baby's needs.
Treatment: The Path to Repair
After birth, your baby will be cared for in the neonatal intensive care unit (NICU). The team’s first goals are to protect the exposed organs with a sterile covering, ensure your baby is stable, and assess their condition to determine the best treatment plan.
Primary Repair
For a small omphalocele, surgeons may perform a single operation within a few days of birth. In this procedure, the organs are placed back into the abdominal cavity, and the opening in the muscle and skin is closed. This direct approach is ideal when the abdomen is large enough to accommodate the organs without causing pressure.
Staged Repair
If the omphalocele is large and the baby’s abdomen is too small, the repair is done in stages. Surgeons place a protective pouch, or "silo," over the organs. Over several days or weeks, the silo is gradually tightened, gently guiding the organs back into the growing abdominal cavity. A final surgery is performed to remove the silo and close the abdominal wall.
Delayed Closure (Paint and Wait)
This non-surgical initial approach is often used for giant omphaloceles to avoid placing too much stress on a newborn. The care team teaches parents how to apply special creams and dressings to the sac, which encourages the baby's skin to slowly grow over the protrusion. This process can take several months. The final surgery to repair the abdominal muscles is scheduled when the child is older and stronger, typically around one to two years of age.
Navigating Life After Surgery: Long-Term Health
The journey with omphalocele continues long after the initial surgeries. While the outlook for most children is excellent, ongoing care helps families manage potential challenges as their child grows.
Breathing and Lung Health
Because the abdominal cavity may be smaller than usual, there is less room for the lungs to fully develop. Many babies, especially those with larger defects, need breathing support like oxygen for a time. You might notice your child breathes a bit faster, particularly with exertion. A pediatric pulmonologist will monitor their lung function to ensure their respiratory system matures properly, allowing them to lead a fully active life.
Feeding and Digestive Wellness
Feeding can be a challenge after leaving the NICU, and some babies may temporarily need a feeding tube to get enough nutrition. Gastroesophageal reflux (GERD) is also common but can be managed with guidance from a gastroenterologist. Parents should also be aware of the small risk of a future bowel obstruction from scar tissue. Seek immediate medical care for signs like sudden green vomiting, abdominal swelling, or inconsolable crying.
Abdominal Strength and Recovery
Your child's surgical scar is a reminder of their strength. While the repaired abdominal wall has a higher risk of developing a hernia—a bulge that may need another surgery—your surgical team will monitor this during follow-up appointments. Children with repaired omphaloceles are not fragile. They go on to crawl, walk, and run just like other kids, enjoying full and active lives.
Building Your Support System
Receiving an omphalocele diagnosis is an emotional experience. Navigating a complex health journey is challenging, but strong support networks are available to empower your family.
Your Multidisciplinary Care Team
You are not alone. A coordinated team of specialists will support your child for years. Many hospitals offer fetal care centers that bring everyone together—maternal-fetal medicine doctors, pediatric surgeons, cardiologists, pulmonologists, nurses, and social workers. This collaborative approach streamlines care and ensures every aspect of your child's health is monitored by an expert.
The Power of Peer Support
Connecting with other parents who have walked this path can be a lifeline. Online communities and support groups provide a safe space to ask practical questions, share fears, and celebrate triumphs. Seeing older children thriving with their "O" offers a powerful sense of hope and perspective that medical teams alone cannot provide.
The Transition from NICU to Home
Moving from the highly structured NICU environment to home can feel daunting. Hospital staff will teach you how to manage any necessary equipment, like feeding tubes or oxygen, before discharge. Taking over this care can feel overwhelming. Lean on home health nursing support and never hesitate to call your care team with questions. They expect your calls and are there to help you adjust to your new role with confidence.