The Evolution of Surgery for Marfan Syndrome: Answering the Aortic Risk
Marfan syndrome is a genetic disorder affecting the body's connective tissue, leading to a range of health issues. While it can impact the eyes, skeleton, and lungs, the most life-threatening complication involves the aorta—the body's largest artery. The weakened aortic wall is prone to dangerous enlargement (aneurysm), which can lead to a tear (dissection) or rupture.
For decades, the central goal of Marfan syndrome management has been to prevent this catastrophic event. This has driven a profound evolution in surgical care, moving from reactive repairs to highly sophisticated, proactive procedures. Today, advancements in surgical techniques and diagnostic imaging have fundamentally changed the prognosis and quality of life for individuals with this condition.
Modern Surgical Advancements: A New Standard of Care
The most significant progress in treating the Marfan aorta lies in developing techniques that are not only safer but also better for the patient's long-term well-being. The focus has shifted from simply replacing damaged tissue to preserving the patient's own anatomy whenever possible.
Valve-Sparing Aortic Root Replacement
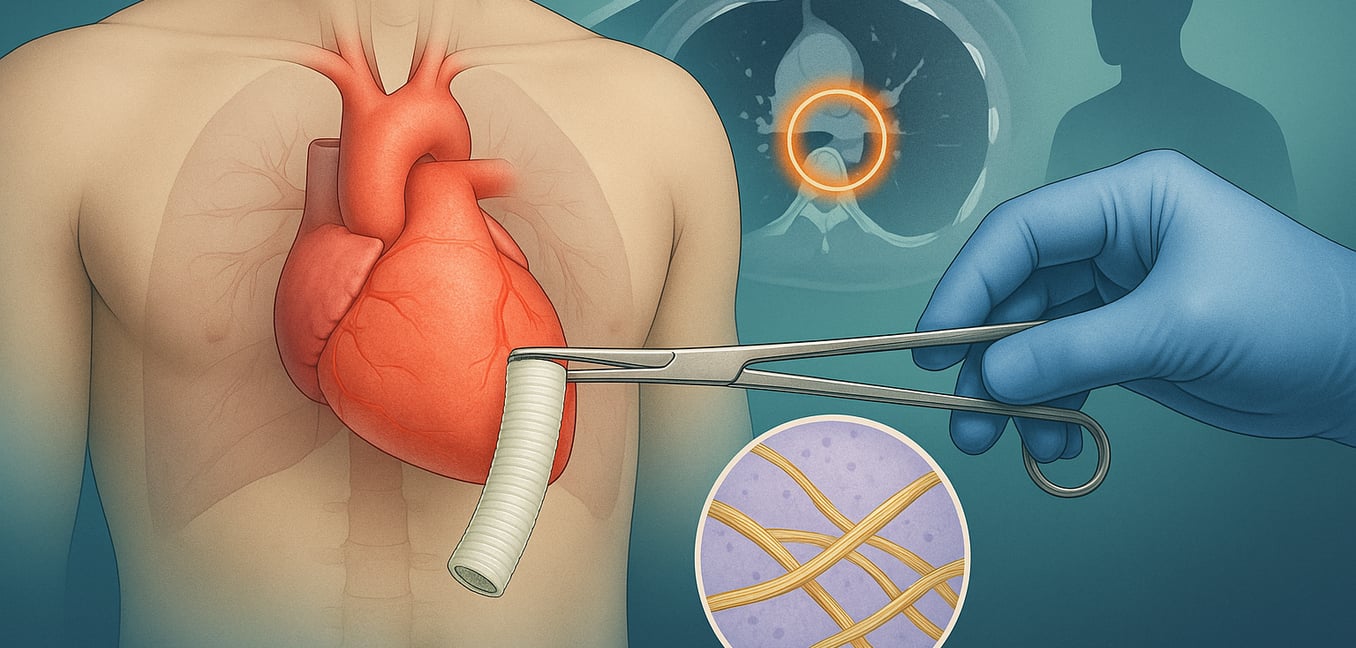
The most transformative development is valve-sparing aortic root replacement, a procedure that preserves the patient’s own aortic valve. This technique directly addresses the aortic aneurysm while avoiding the lifelong complications associated with prosthetic valves.
- The David Procedure: The most common valve-sparing technique is the re-implantation or "David" procedure. A surgeon carefully separates the patient's healthy aortic valve from the enlarged aorta. The weakened aorta is then replaced with a synthetic graft, and the patient's own valve is meticulously secured inside this new, durable housing.
- Exceptional Durability: This repair is highly durable, with studies showing a low failure rate of just 5-7% at 10 years post-surgery. This offers young patients the potential for a single, lifelong cardiac repair, freeing them from the certainty of future re-operations associated with tissue valves.
- Freedom from Blood Thinners: Crucially, preserving the native valve frees patients from the lifelong need for anticoagulant medications. This eliminates the constant risk of bleeding complications and removes the daily burden of managing these drugs, significantly improving quality of life.
The Role of Advanced Imaging in Surgical Planning
Modern surgery is guided by incredibly detailed pre-operative planning, made possible by advanced imaging technologies. Cardiac computed tomography (CT) and cardiovascular magnetic resonance (CMR) provide a precise roadmap of a patient's anatomy, revolutionizing how surgeons prepare for these complex operations.
- Personalized Surgical Timing: Advanced imaging allows doctors to use personalized metrics to determine the right time for surgery. By comparing the aorta's size to the patient's overall body size, they can identify a clear risk threshold, moving from subjective judgment to data-driven decisions for proactive intervention.
- 3D Anatomical Models: Surgeons can create interactive 3D models of the aorta. These virtual maps allow them to rehearse the procedure, select the perfectly sized graft, and plan the safest surgical approach, which helps reduce operating time and minimize surprises in the operating room.
- Comprehensive Aortic Scans: Imaging provides a head-to-toe view of the entire aorta, not just the root. This allows surgeons to identify other weak spots in the aortic arch or descending aorta that may need to be addressed, enabling a more definitive, single-stage repair.
- Precise Coronary Mapping: ECG-gated CT scans create crystal-clear images of the coronary arteries. Knowing their exact location and path is critical for the surgeon, who must detach and re-implant them into the new graft, helping to prevent life-threatening complications.
How Surgery Has Evolved: The Traditional Approach and Its Drawbacks
To fully appreciate today's advancements, it is important to understand the traditional surgical methods they replaced. For many years, the standard procedure was a composite aortic root replacement, which came with significant lifelong trade-offs.
This operation involved replacing the enlarged section of the aorta and the patient’s aortic valve with a single unit—a synthetic tube graft with a prosthetic valve pre-attached. While effective at preventing aortic rupture, it forced patients into a difficult choice between two imperfect valve options.
- Mechanical Valves: Made from durable materials like carbon, these valves are designed to last a lifetime. However, they require patients to take lifelong anticoagulant (blood-thinning) medications to prevent dangerous blood clots, which introduces a constant risk of major bleeding.
- Biologic (Tissue) Valves: Typically made from animal tissue, these valves do not require long-term anticoagulation. Their major downside is a limited lifespan; they degenerate over 10 to 15 years, necessitating high-risk re-operations, a major concern for younger patients.
The development of valve-sparing techniques was a direct response to these challenges, offering a solution that provides the durability of a mechanical valve without the need for blood thinners, marking a true paradigm shift in Marfan care.