What Foods Should You Avoid with VLCAD Deficiency?
Living with Very Long-Chain Acyl-CoA Dehydrogenase (VLCAD) deficiency means paying close attention to your diet, particularly the types and amounts of fats you consume. This genetic condition affects how your body breaks down certain fats for energy. Understanding which foods to limit or avoid is crucial for managing VLCAD and maintaining your health.
First, What is VLCAD Deficiency?
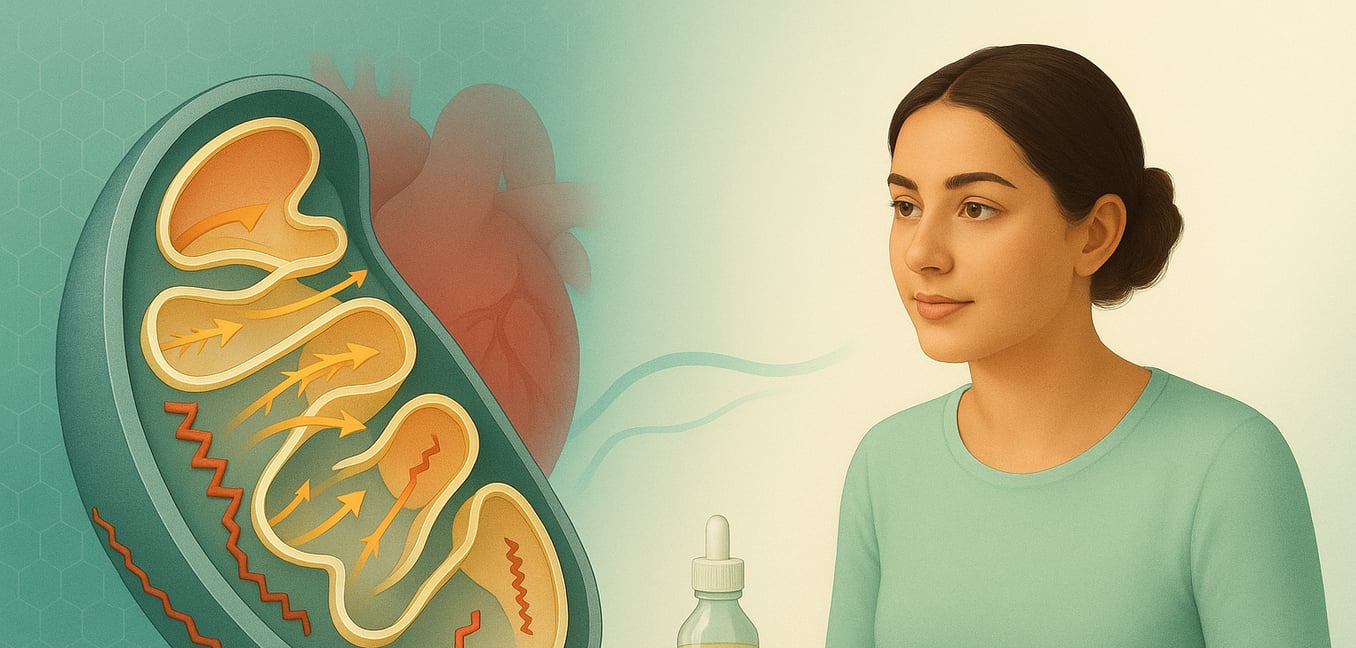
VLCAD deficiency is an inherited metabolic disorder. It stems from changes in the ACADVL gene, which holds the instructions for making an enzyme essential for breaking down specific fats called very long-chain fatty acids (LCFAs).
- Inheritance: To have VLCAD, a person usually needs to inherit an altered gene from both parents. Individuals with only one altered gene are "carriers"; they typically do not show symptoms but can pass the gene to their children.
- Energy Production Problem: Our bodies use LCFAs as a key energy source, especially during periods of fasting (not eating) or illness. In VLCAD deficiency, the enzyme needed to process these fats is faulty or missing. This means LCFAs cannot be effectively converted into energy.
- Consequences: This energy shortage can lead to serious issues like low blood sugar (hypoglycemia) and extreme tiredness (lethargy). Furthermore, these unprocessed LCFAs can accumulate in vital organs such as the heart, liver, and muscles, potentially causing damage like heart muscle disease (cardiomyopathy), impaired liver function, or muscle weakness over time.
- Varying Severity: VLCAD deficiency impacts individuals differently. Some infants experience a severe, early-onset form with serious heart problems. A childhood-onset form might involve liver issues and low blood sugar. The late-onset form, appearing in adolescence or adulthood, usually causes milder, muscle-related symptoms often triggered by exercise, illness, or fasting.
The Core Dietary Strategy: Limiting Long-Chain Fatty Acids
The central principle of a VLCAD diet is to restrict foods high in long-chain fatty acids. Since your body cannot properly metabolize these fats, avoiding them helps prevent their harmful buildup and the associated energy crisis.
Key Food Categories to Limit or Avoid:
-
Fatty Meats:
These are significant sources of LCFAs.
- Examples: Bacon, sausage, salami, fatty cuts of beef (like ribeye, brisket), lamb, and pork (like pork belly, ribs). Processed meats often contain hidden fats.
-
Full-Fat Dairy Products:
Whole milk and products made from it are rich in LCFAs.
- Examples: Whole milk, heavy cream, butter, most cheeses (especially hard and creamy varieties), full-fat yogurt, and ice cream.
-
Certain Oils and Fats:
Many common cooking oils and solid fats are high in LCFAs.
- Examples: Butter, lard, shortening, coconut oil, palm oil, and palm kernel oil. While some vegetable oils (like olive or canola) might be used in moderation under guidance, high-fat dressings and sauces made with problematic oils should be limited.
-
Fried Foods:
Foods cooked by deep frying absorb large amounts of oil, significantly increasing their LCFA content.
- Examples: French fries, fried chicken, doughnuts, and other deep-fried snacks or meals.
-
Nuts and Seeds (in large quantities):
While offering some health benefits, many nuts and seeds are dense in fats, including LCFAs.
- Examples: Almonds, walnuts, pecans, peanuts, cashews, and their respective butters. Small, carefully measured amounts might be permissible for some individuals under dietetic supervision.
-
Processed and Packaged Foods:
Many commercially prepared foods contain hidden LCFAs.
- Examples: Pastries, cookies, cakes, crackers, chocolate, and many convenience meals. Reading labels is essential.
Why This Restriction is Crucial:
Consuming foods rich in LCFAs when you have VLCAD deficiency can lead to:
- Metabolic Crises: An inability to convert these fats into energy, especially when your body needs it most (like during illness or fasting), can trigger a metabolic crisis. Symptoms include severe lethargy, irritability, and dangerously low blood sugar.
- Organ Damage: The accumulation of unprocessed LCFAs in the heart, liver, and muscles can cause long-term complications.
The Role of Medium-Chain Triglycerides (MCTs):
To help meet energy needs while restricting LCFAs, individuals with VLCAD are often prescribed medical foods or oils containing medium-chain triglycerides (MCTs). MCTs are metabolized differently and provide a more accessible energy source for those with VLCAD. Your metabolic dietitian will determine the appropriate amount of MCT oil or MCT-containing formula for your specific needs. This is not a fat to be found in regular foods but a prescribed supplement.
Personalized Dietary Limits for Long-Chain Fatty Acids
While the general advice is to avoid high-LCFA foods, the specific amount of LCFAs allowed in your diet is not universal. It is carefully personalized by your healthcare team, including a metabolic physician and dietitian.
- Factors Influencing Limits: Your age, the severity of your VLCAD (mild, moderate, or severe), your current health status, lab results, and whether you are experiencing symptoms all play a role in determining your LCF target.
- Typical Ranges: For instance, infants with severe VLCAD might have very strict LCF restrictions, sometimes allowing only a few grams per day or a small percentage of total energy from LCFAs. Older individuals or those with milder forms might have a plan allowing more LCFAs, but always with careful monitoring.
- Dynamic Adjustments: These dietary recommendations are not static. Your medical team will adjust them based on your growth (for children), health changes, lab results, and symptom control throughout your life.
The Critical Importance of Avoiding Prolonged Fasting
For individuals with VLCAD deficiency, going without food for extended periods (fasting) poses significant health risks. This is because when the body is deprived of immediate energy from food, it naturally tries to break down stored fats, including LCFAs.
- Trigger for Metabolic Crisis: Since VLCAD impairs the breakdown of LCFAs, fasting can quickly lead to an energy shortage. This is especially true during illness, fever, or intense physical activity, which increase the body's energy demands. Such a shortage can precipitate a metabolic crisis.
-
Age-Specific Fasting Guidelines:
Healthcare providers establish strict, individualized limits on how long individuals with VLCAD can safely fast. These guidelines are crucial for ensuring a continuous supply of accessible energy.
- Newborns and young infants might need to feed every 3 to 4 hours.
- Older children (e.g., over 12 months) might tolerate 8 to 12 hours of fasting when well, but this varies.
- Adults also have specific fasting limits, especially overnight or if a meal is missed.
- A Universal Precaution: The need to avoid prolonged fasting applies to everyone with VLCAD, regardless of the severity of their condition or whether they are usually symptom-free. The underlying metabolic issue is always present. Regular food intake, as per medical advice, is a fundamental safety measure.
Strategic Eating: Meal Timing and Carbohydrate Intake
Beyond just avoiding certain fats and prolonged fasts, how and when you eat, particularly carbohydrates, is vital for managing VLCAD. The goal is to maintain a steady supply of usable energy, reducing the body's need to access its compromised fat metabolism pathways.
- Consistent Carbohydrate Intake: Carbohydrates become a primary fuel source. Regular meals and snacks rich in appropriate carbohydrates help maintain stable blood sugar levels and prevent hypoglycemia. This consistent fueling protects muscles and vital organs.
-
Uncooked Cornstarch (UCCS):
Some individuals with VLCAD, particularly those prone to hypoglycemia during fasting, may be prescribed uncooked cornstarch. UCCS is a slow-digesting carbohydrate that provides a gradual release of glucose.
- Its use is not universal and depends on individual needs, age, VLCAD severity, and documented hypoglycemia.
- The decision to use UCCS should always be made in close consultation with your metabolic team.
- Tailored Meal Plans: Your metabolic physician and dietitian will develop a personalized meal plan. This plan will consider your specific VLCAD type, age, risk of hypoglycemia, fasting tolerance, and overall dietary needs to ensure you receive adequate energy safely and effectively. Regular communication with your healthcare team is essential to adjust this plan as your needs change.
Managing VLCAD deficiency requires a lifelong commitment to specific dietary strategies. By understanding which foods to avoid, adhering to safe fasting guidelines, and working closely with your healthcare team, you can effectively manage the condition and support your overall health.