Treatments for Marfan Syndrome
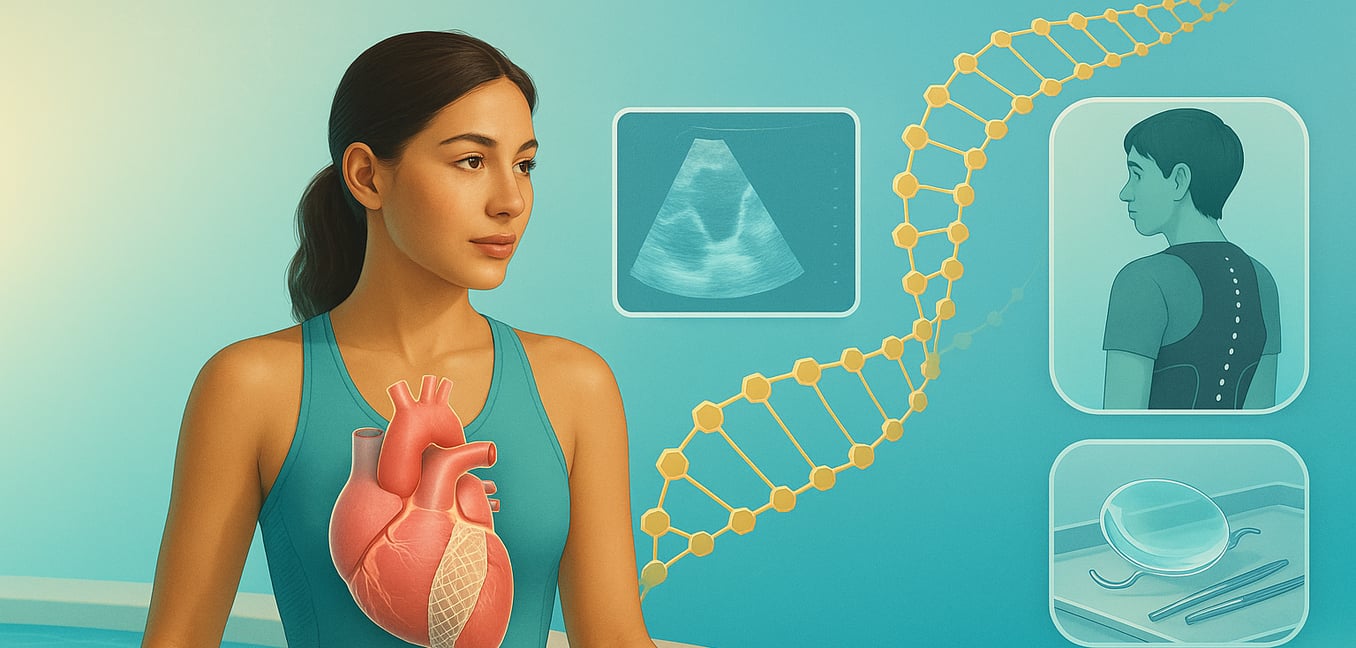
Marfan syndrome is a genetic disorder affecting the body's connective tissue—the "glue" that supports our organs, bones, and blood vessels. Caused by a flaw in the gene for fibrillin-1, this condition weakens structures throughout the body. While it can cause skeletal issues like a curved spine and eye problems like a dislocated lens, the most serious risk involves the aorta, the main artery from the heart. The weakened aortic wall can stretch and bulge, creating an aneurysm that could lead to a life-threatening tear. Therefore, treatments for Marfan syndrome focus on managing these symptoms and proactively protecting the aorta to prevent severe complications.
Cardiovascular Management
The primary focus of Marfan syndrome treatment is protecting the heart and aorta from the effects of weakened connective tissue. Management involves a two-pronged approach: daily medical therapy to reduce stress on the aorta and surgical intervention to prevent a catastrophic rupture.
Medication and Monitoring
Day-to-day management relies on a combination of medications and consistent imaging to slow aortic enlargement and track any changes. This proactive strategy is the first line of defense.
- Protective Medications: Doctors typically prescribe medications like beta-blockers or angiotensin receptor blockers (ARBs). These drugs work by lowering blood pressure and reducing the force of each heartbeat, which lessens the daily strain on the fragile aortic wall. Consistent use is crucial to slow the rate of aortic stretching.
- Regular Imaging: Frequent check-ups using echocardiograms (heart ultrasounds) and sometimes CT or MRI scans are essential. These tests provide precise measurements of the aorta's diameter, allowing the medical team to track its growth over time. This data is the key factor in deciding the right time for preventative surgery.
- Aortic Valve Assessment: The same weakness that affects the aorta can cause the aortic valve leaflets to become floppy and leak, a condition called aortic insufficiency. Regular echocardiograms also monitor the valve's function, as its health is a critical factor in planning any potential surgery.
Surgical Intervention
When medication is not enough to halt the aorta's expansion, surgery becomes necessary to prevent a life-threatening dissection or rupture. The goal is to intervene proactively before an emergency occurs, typically when the aortic root reaches a diameter of around 4.5 to 5.0 centimeters.
- Valve-Sparing Aortic Root Replacement: This is often the preferred surgical option if the patient's aortic valve is still healthy. In this procedure, known as the David operation, the surgeon replaces the enlarged section of the aorta with a synthetic graft and carefully re-implants the patient's own valve inside it. The primary benefit is avoiding the need for lifelong blood-thinning medication.
- Traditional Aortic Root Replacement: If the aortic valve is too damaged or leaky to be saved, the surgeon will replace both the weakened aorta and the valve with a composite graft. Patients must then choose between a mechanical valve, which is highly durable but requires lifelong anticoagulation therapy (blood thinners) like warfarin to prevent blood clots, or a biological (tissue) valve, which does not require anticoagulants but may wear out and need replacement in the future.
Skeletal and Ocular Therapies
While cardiovascular health is the top priority, a comprehensive care plan also addresses the effects of Marfan syndrome on the skeletal system and eyes to improve quality of life and preserve function.
- Spinal Curvature: Doctors monitor for scoliosis (a sideways curve of the spine) or kyphosis (a forward hunch), especially during growth spurts. Treatment ranges from observation for mild curves to a custom back brace to halt progression in growing children. Severe curves that cause pain or impact lung function may require spinal fusion surgery.
- Vision Problems: Routine exams with an ophthalmologist are critical for detecting issues like ectopia lentis (dislocation of the eye's lens). This is often managed with specialized glasses or contact lenses. If the dislocation is severe or causes complications like cataracts, surgery to remove the natural lens and implant an artificial one may be necessary to restore clear vision.
- Chest Deformities: A sunken chest (pectus excavatum) or protruding chest (pectus carinatum) is common. These are often only a cosmetic concern. However, if a sunken chest is severe enough to compress the heart and lungs and cause shortness of breath, corrective surgery can be performed to relieve pressure and improve function.
Lifestyle Adjustments
Beyond medical and surgical treatments, certain lifestyle modifications are essential for protecting the aorta from unnecessary stress. These adjustments are a key part of long-term self-management. It is crucial to avoid activities that cause sudden spikes in blood pressure, including:
- High-intensity competitive sports.
- Contact sports like football or hockey.
- Strenuous activities like heavy weightlifting or straining.
Instead, individuals are encouraged to engage in low-to-moderate intensity aerobic exercises, such as walking, swimming, or cycling, to maintain cardiovascular fitness safely. A cardiologist can help develop a personalized exercise plan that balances an active lifestyle with the need to protect the aorta.