Understanding Succinic Semialdehyde Dehydrogenase Deficiency
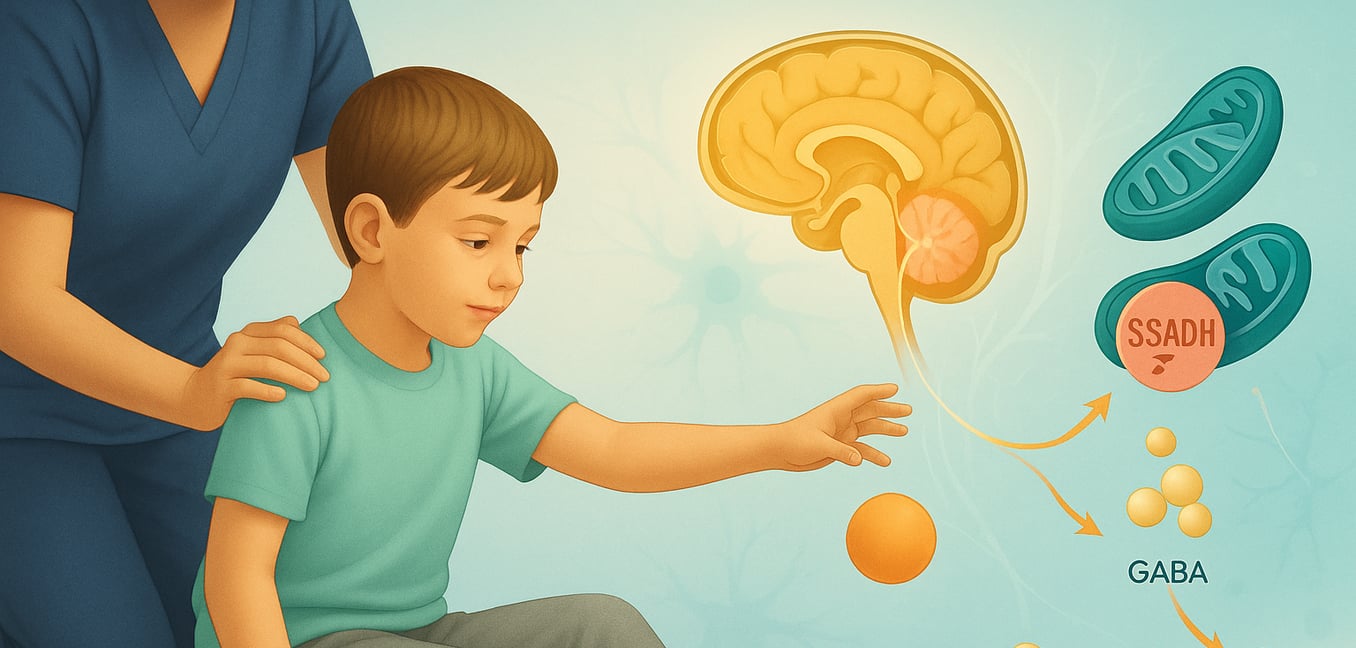
Succinic semialdehyde dehydrogenase (SSADH) deficiency is a rare, inherited metabolic disorder. It affects the body's process for breaking down gamma-aminobutyric acid (GABA), a key chemical messenger in the brain. This breakdown issue leads to the buildup of other substances, notably gamma-hydroxybutyric acid (GHB), which can result in a range of neurological problems. Awareness of this condition's core aspects is vital for affected individuals, their families, and healthcare teams.
Key characteristics of SSADH deficiency are:
- General Clinical Impact: This disorder typically manifests in early childhood as a neurological condition that may progress slowly or remain static. It broadly affects development, movement, and behavior, with specific symptoms and severity varying significantly among individuals.
- Underlying Cause: SSADH deficiency is an autosomal recessive condition, meaning a child must inherit a non-working copy of the ALDH5A1 gene from both parents. This gene provides instructions for making the SSADH enzyme. When this enzyme is deficient, GABA metabolism is disrupted, causing succinic semialdehyde to accumulate and convert into GHB, which builds up in body fluids and is thought to cause neurological symptoms.
- Diagnosis: Identifying SSADH deficiency involves specific laboratory tests and brain imaging. A key indicator is elevated GHB levels in urine, detected by organic acid analysis (a test for unusual chemicals in urine). Reduced SSADH enzyme activity can be confirmed in lymphocytes (a type of white blood cell). Brain MRI scans often reveal signal changes in areas like the globus pallidi (specific regions deep within the brain). A definitive diagnosis is made through molecular genetic testing that identifies mutations in both copies of the ALDH5A1 gene.
- Management Approach: Currently, there is no cure for the enzyme deficiency itself. Treatment focuses on managing symptoms. Medications like carbamazepine and lamotrigine can help control seizures, while other drugs may address neurobehavioral issues such as anxiety or hyperactivity. Supportive therapies, including physical, occupational, and speech therapy, are essential for improving daily functioning and enhancing the quality of life.
Early Symptoms: Developmental and Motor Skill Challenges
The initial signs of SSADH deficiency commonly emerge during infancy or early childhood, often becoming apparent as a child misses or is slow to reach expected developmental milestones. These early symptoms frequently involve physical development and the acquisition of motor skills.
- Delayed Motor Milestones: Children with SSADH deficiency often take longer than their peers to achieve fundamental physical skills. This can include delays in gaining head control, sitting independently, crawling, pulling to a stand, or walking. The extent of these delays can range from mild to significant.
- Hypotonia (Reduced Muscle Tone): Many infants and young children exhibit hypotonia, meaning their muscles have less tension, making them feel 'floppy.' This can affect activities requiring muscle strength, such as holding up the head, feeding effectively, or maintaining posture, and contributes to motor skill delays.
- Ataxia (Impaired Coordination): Some children display ataxia, which is difficulty coordinating voluntary movements. This may manifest as unsteadiness in sitting, crawling, or walking, making movements appear clumsy or jerky. Fine motor skills, like grasping objects, can also be affected. In SSADH deficiency, ataxia is often non-progressive and may sometimes improve with therapy.
- Language and Speech Delays: Significant delays in language and speech are common. This can range from reduced babbling in infancy to limited vocabulary or difficulty forming words and sentences in toddlerhood. Expressive language (speaking) is often more affected than receptive language (understanding).
Impact on Neurological Function and Cognitive Abilities
SSADH deficiency has a profound impact on brain function, leading to various neurological and cognitive challenges that often become more evident as individuals age. These effects extend beyond initial motor and speech difficulties.
Key areas impacted include:
- Intellectual Disability and Cognitive Deficits: A wide range of intellectual disability, from mild to severe, is common. Individuals may learn at a slower pace and face challenges with complex information or academic skills. Cognitive deficits can also affect executive functions like planning and organization.
- Seizures (Epilepsy): Over half of those with SSADH deficiency experience seizures, with the likelihood increasing with age. Seizures can present in various forms, including generalized tonic-clonic or atypical absence types. For older individuals, there's a noted risk of Sudden Unexpected Death in Epilepsy (SUDEP), emphasizing the need for careful seizure management.
- Sleep Disturbances: Problems with sleep are frequently reported. These can include excessive daytime sleepiness (somnolence), particularly in younger individuals, or difficulties falling asleep and staying asleep at night. Poor sleep can worsen irritability and behavioral issues.
Behavioral and Psychiatric Manifestations
Individuals with SSADH deficiency often experience a complex array of behavioral and psychiatric symptoms. These stem from the disorder's impact on brain chemistry and can significantly influence daily life, social interactions, and overall well-being, often evolving with age.
- Attention Difficulties and Hyperactivity: Symptoms similar to Attention Deficit Hyperactivity Disorder (ADHD) are prevalent, especially in childhood. These include significant inattention, difficulty sustaining focus, and excessive physical restlessness (hyperkinesis), which can make learning challenging.
- Anxiety, Obsessive-Compulsive Traits, and Repetitive Behaviors: Anxiety is common, presenting as excessive worry or social unease. Individuals may also develop obsessive-compulsive disorder (OCD)-like symptoms, such as recurrent intrusive thoughts and repetitive behaviors (e.g., frequent rocking), which can become more pronounced over time.
- Challenges with Mood and Behavioral Regulation: Difficulties managing mood and behavior can lead to heightened irritability, easy agitation, or aggressive episodes. In some cases, self-injurious actions may occur, requiring multifaceted behavioral therapies and a supportive environment.
- Psychotic Features and Altered Perceptions: Less commonly, some individuals, particularly in adolescence or adulthood, may experience more severe psychiatric symptoms such as hallucinations (seeing or hearing things that are not there). The onset of such features requires careful psychiatric evaluation and management.
Additional Common Symptoms and Individual Variability
Beyond the primary neurological and behavioral challenges, SSADH deficiency can present with other physical signs. The specific symptoms and their severity can differ markedly from one person to another, even within the same family, highlighting the disorder's diverse nature.
This variability extends to several other commonly observed features:
- Hyporeflexia (Decreased or Absent Reflexes): Many individuals have hyporeflexia, where reflex responses (like the knee-jerk) are weaker or absent. This indicates an impact on the nerve pathways controlling automatic muscle reactions and is a clinical sign used in neurological assessment.
- Ocular (Eye) Abnormalities: Eye-related issues can occur, varying in type and severity. These may include nystagmus (involuntary, rapid eye movements), oculomotor apraxia (difficulty intentionally moving the eyes to follow an object), or generally poor vision, potentially impacting visual learning and daily tasks.
- Variations in Head Size (Craniofacial Differences): Some individuals may show differences in head size, such as an unusually small head (microcephaly) or, less commonly, an unusually large head (macrocephaly). These variations can be noted during routine pediatric measurements.
- Significant Intrafamilial Variability: A noteworthy aspect of SSADH deficiency is the considerable variation seen even among siblings with the same ALDH5A1 gene mutations. One sibling might have severe developmental delays and frequent seizures, while another with the same genetic changes could have much milder symptoms. This suggests that other genetic or environmental factors likely modify the disease's expression, underscoring the need for personalized care.