Neuroblastoma is a childhood cancer that arises from developing nerve cells, most often affecting infants and children under five. The disease is known for its highly variable behavior; some tumors may disappear on their own, while others are incredibly aggressive. To guide treatment, doctors classify neuroblastoma into low, intermediate, or high-risk groups. While factors like a child’s age and tumor location play a role, a high-risk diagnosis is primarily driven by two key characteristics: aggressive tumor genetics and the cancer's spread to other parts of the body (metastasis). This article will explore these two defining factors in detail.
For context, low-risk neuroblastoma has an excellent prognosis, often requiring only surgery or even just observation. Intermediate-risk neuroblastoma requires more treatment, typically surgery and chemotherapy, but survival rates remain very high. High-risk neuroblastoma, however, is a fundamentally different disease that requires a far more intensive and complex approach to treatment.
The Genetic Driver: MYCN Amplification
One of the most critical factors in determining neuroblastoma risk is the status of a gene called MYCN. While this gene plays a normal role in cell development, in some neuroblastoma tumors, it becomes "amplified," acting as a powerful engine that drives aggressive cancer growth.
Gene amplification means that instead of the normal two copies of the MYCN gene, the cancer cells have created many extra copies. Imagine a faulty copy machine stuck in the "on" position, churning out hundreds of duplicates of the same page. This flood of extra gene copies leads to a massive overproduction of the MYCN protein, which acts like a gas pedal stuck to the floor. It sends overwhelming signals for cancer cells to grow and divide relentlessly, ignoring the body’s natural stop signals.
The presence of MYCN amplification is a defining feature of high-risk neuroblastoma and has a profound impact on a child's prognosis. Tumors with this genetic change are inherently more aggressive, grow faster, and are more likely to have already spread by the time of diagnosis. Because of its significance, testing for MYCN amplification is a standard and essential part of the diagnostic process for every child with neuroblastoma. A finding of MYCN amplification almost always places a child in the high-risk category, signaling the need for the most aggressive treatment available.
The Physical Spread: Metastasis
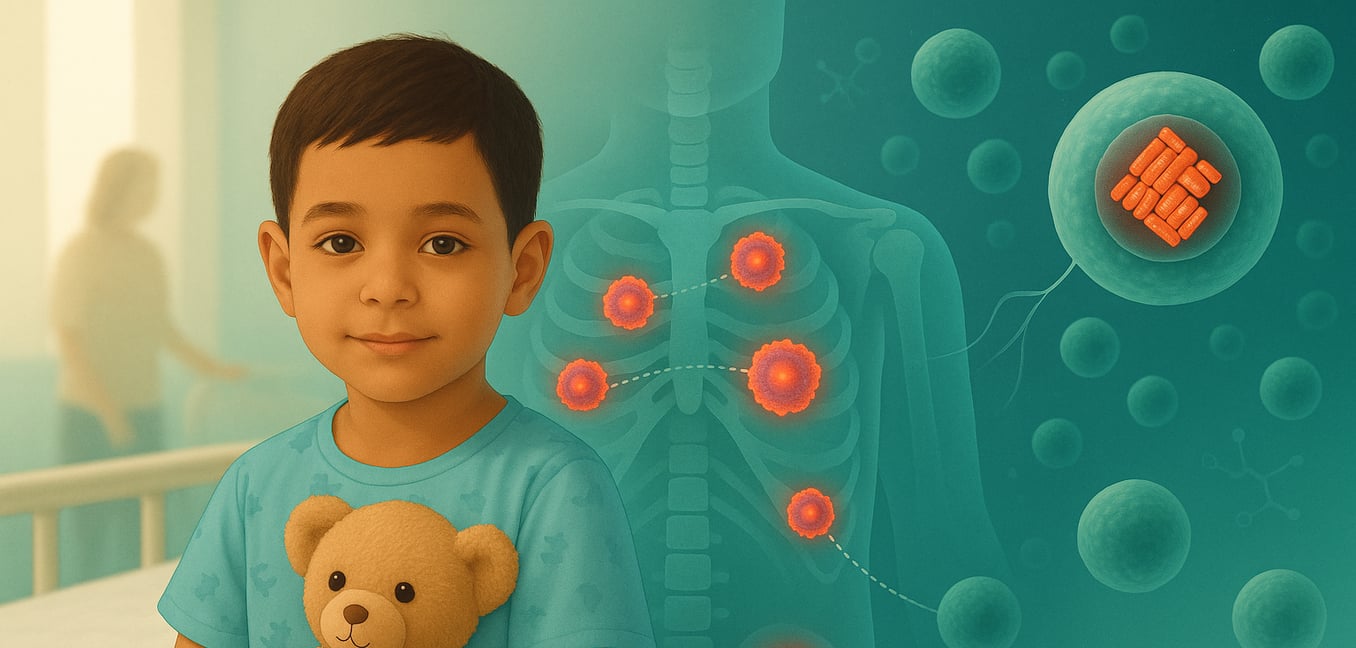
Beyond aggressive genetics, the physical spread of cancer is the other primary characteristic of high-risk neuroblastoma. This process, known as metastasis, occurs when cancer cells break away from the original tumor and travel through the bloodstream or lymphatic system to form new tumors in distant parts of the body. The presence of metastatic disease at diagnosis immediately classifies the cancer as advanced and is a key reason a child is assigned to the high-risk group.
A major challenge of neuroblastoma is that for a majority of children—approximately 70%—the cancer has already spread by the time it is discovered. This means the fight is not against a single tumor in one location, but against cancer that has established itself in multiple areas. This reality demands a systemic, body-wide treatment approach to target cancer cells wherever they may be hiding.
Neuroblastoma cells tend to travel to specific locations, most commonly the bones, bone marrow, liver, and distant lymph nodes. When cancer infiltrates the bone marrow, it can disrupt the production of healthy blood cells, while spread to the bones can cause significant pain. To map the extent of the disease, doctors use specialized imaging. A meta-iodobenzylguanidine (MIBG) scan is a key tool that uses a radioactive tracer that acts like a magnet for neuroblastoma cells. This tracer is absorbed by the cancer, causing the primary tumor and any metastatic sites to "light up" during the scan, giving doctors a clear map of the disease. A bone marrow biopsy is also performed to check for cancer cell infiltration in this common site of spread.
Prognosis for High-Risk Neuroblastoma
For families facing a high-risk diagnosis, the prognosis can be difficult to process. While survival rates have improved dramatically over the decades, the outlook remains serious, with the overall five-year survival rate currently around 50%. This statistic, however, is a historical average and not a definitive prediction for any individual child. It reflects the immense challenge of the disease, but also the fact that modern therapies give about half of these children a chance to be cured.
A crucial factor influencing an individual’s prognosis is how well their cancer responds to the initial phase of treatment, known as induction chemotherapy. Doctors use imaging scans to carefully monitor the tumor's size and the extent of metastasis after the first rounds of therapy. A significant reduction in the tumor and the clearing of cancer from distant sites are very positive signs, suggesting the cancer is sensitive to the drugs being used.
The prognosis is a constantly evolving picture due to rapid advances in treatment. The statistics from even a few years ago may not fully capture the potential of today's therapies, as ongoing research continues to improve outcomes. This means the 50% survival rate should be seen as a historical benchmark, not a fixed ceiling for a child diagnosed today.
Why High-Risk Treatment Is So Intense
Tackling high-risk neuroblastoma requires one of the most intensive and lengthy treatment plans in pediatric oncology, often spanning 18 months or more. This multi-stage approach is necessary to combat a cancer that is both widespread and biologically resilient due to factors like MYCN amplification. The treatment is a carefully orchestrated sequence of four main phases.
Phase 1: Induction Chemotherapy and Surgery
The first phase is a powerful initial assault on the cancer using multiple rounds of high-dose chemotherapy. The goals are to shrink the primary tumor and, just as importantly, clear cancer cells that have spread to the bone marrow and other metastatic sites. Following chemotherapy, a surgeon performs a complex operation to remove as much of the primary tumor as possible. During this phase, the child’s own healthy stem cells are also collected from their blood and frozen for later use.
Phase 2: Consolidation with Stem Cell Transplant
Next is the consolidation phase, arguably the most grueling part of treatment. The child receives myeloablative chemotherapy—doses so high they destroy the bone marrow—to eliminate any microscopic, drug-resistant cancer cells that survived the initial attack. The child is then "rescued" with an infusion of their previously collected stem cells. This process, an autologous stem cell transplant, allows their body to regrow a healthy bone marrow and immune system.
Phase 3: Radiation Therapy
After the body has recovered from the transplant, radiation therapy is used to target the area where the primary tumor was located. This acts as a crucial "clean-up" step, delivering focused energy beams to destroy any residual cancer cells that might have been left behind after surgery. This helps prevent the cancer from recurring in its original location, a problem known as local relapse.
Phase 4: Maintenance and Immunotherapy
The final stage of treatment is designed to keep the cancer from returning by targeting any dormant cells that might still be hiding in the body. This phase prominently features immunotherapy using anti-GD2 antibodies, a treatment that helps the child's newly rebuilt immune system recognize and destroy neuroblastoma cells. This is often combined with an oral medication, isotretinoin, which encourages any remaining cancer cells to mature into harmless tissue, providing another layer of defense against relapse.