The Genetic Roots of Amish Lethal Microcephaly
Amish lethal microcephaly (ALM) is a rare and devastating genetic disorder found almost exclusively within Old Order Amish communities. The condition is defined by severe microcephaly, a term for a significantly small head size, which is present at birth and indicates abnormal brain development in the womb. The effects of ALM are profound, leading to severe neurological impairment and a uniformly fatal outcome, typically within the first year of life.
Children born with ALM display a consistent and tragic set of symptoms, including:
- Severe primary microcephaly: A head circumference far below the average for newborns.
- Distinct facial features: A prominent, drooping forehead is a common characteristic.
- Profound developmental failure: This involves severe intellectual disability and a complete lack of developmental milestones.
- Abnormal muscle tone: Infants often have either rigid or floppy limbs.
Understanding the specific genetic error behind this condition is crucial for providing accurate diagnoses and genetic counseling to affected families.
The SLC25A19 Founder Mutation
The direct cause of Amish lethal microcephaly is a specific mutation in the
SLC25A19
gene. This particular error is known as a founder mutation, meaning it was present in one of the early founders of the Old Order Amish population. Due to the community's relative genetic isolation, this mutation has been passed down through generations, making it more common within this group than in the general population.
The specific mutation responsible for ALM is a point mutation designated G177A. This seemingly small change in the genetic code occurs in a critical region of the gene and has catastrophic consequences. It results in a near-total loss of function for the protein the gene is meant to create. Because the developing brain is highly vulnerable to the effects of this protein's absence, the G177A mutation leads to the severe and uniformly fatal outcome seen in ALM.
This condition follows an autosomal recessive inheritance pattern. For a child to be affected, they must inherit one copy of the faulty
SLC25A19
gene from each parent. The parents, who each carry only one faulty copy, are known as carriers. They are typically healthy and show no signs of the disorder, which is why ALM can appear unexpectedly in a family.
The Biological Pathway: How a Faulty Gene Shuts Down the Brain
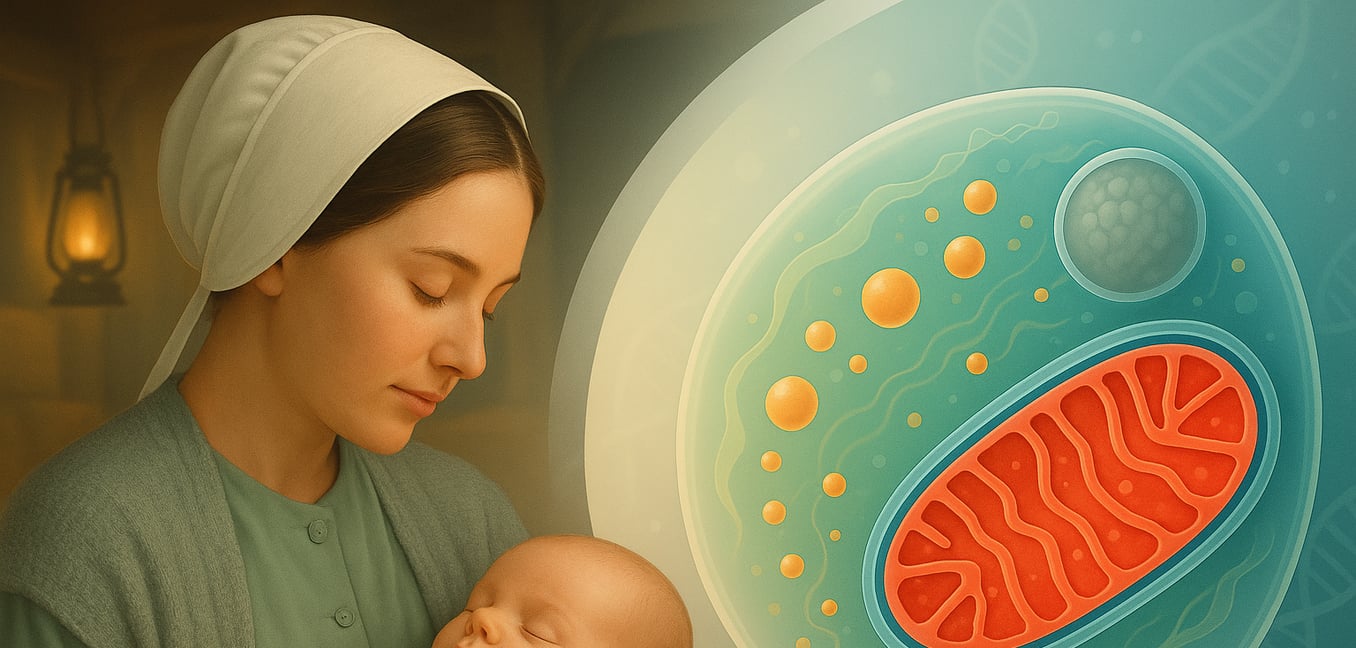
The
SLC25A19
gene contains the instructions for building a mitochondrial transporter protein. This protein has a vital job: it moves a form of vitamin B1, called thiamine pyrophosphate (TPP), into the mitochondria—the cell's powerhouses.
An Energy Crisis in the Developing Brain
The brain is the most energy-demanding organ in the body. During fetal development, neural cells must divide, migrate, and form trillions of connections, a process that requires a massive and constant supply of cellular energy in the form of ATP. Mitochondria produce this ATP, but they cannot do so without essential cofactors like TPP.
When the
SLC25A19
transporter is defective due to the G177A mutation, TPP cannot enter the mitochondria. This creates a severe energy crisis that stalls brain development at its most critical stages. Neural cells cannot divide properly, mature, or form the complex structures of a healthy brain, resulting in severe microcephaly.
Buildup of Toxic Byproducts
The failure of mitochondrial energy production has a second devastating effect. When the cellular energy pathway is blocked, metabolic intermediates that are normally processed get backed up. This leads to a harmful accumulation of substances like alpha-ketoglutaric acid and lactic acid in the body. These compounds are toxic to the developing nervous system, causing direct damage to neurons and worsening the injury already caused by the energy deficit. This combination of energy starvation and cellular toxicity explains the rapid and severe neurodegeneration seen in ALM.
Related Conditions and the Importance of Genetic Diagnosis
While the G177A mutation in
SLC25A19
causes ALM, it is important to understand that other genetic conditions can present with similar features, sometimes even within the same communities. This highlights the concept of genetic heterogeneity, where different genes can cause clinically similar diseases.
Different Mutations, Different Outcomes: THMD4
Other, less severe mutations in the same
SLC25A19
gene cause a related but distinct disorder called thiamine metabolism dysfunction syndrome 4 (THMD4). Unlike the G177A mutation which eliminates protein function, the mutations causing THMD4 only impair it. This allows some TPP to reach the mitochondria, which is enough to prevent the severe microcephaly and early death seen in ALM. Instead, individuals with THMD4 typically experience episodes of brain dysfunction (encephalopathy), often triggered by illness or fever. This is a clear example of a genotype-phenotype correlation, where the specific type of genetic error dictates the clinical outcome.
A Similar Story, A Different Gene: The BRAT1 Founder Mutation
Another important differential diagnosis within some Amish communities is a severe neonatal syndrome caused by mutations in the
BRAT1
gene. Like ALM, this condition can be traced to a founder mutation and is characterized by profound developmental arrest, intractable seizures, and early death. This disorder is caused when a child inherits a faulty copy of the
BRAT1
gene from both parents. The most severe cases are linked to mutations that act like a "stop" signal, preventing the full protein from being made and leading to a complete loss of its function in DNA damage repair.
The clinical overlap between ALM and severe
BRAT1
-related disorders makes diagnosis based on symptoms alone impossible. Accurate genetic testing is therefore essential to identify the precise cause, which allows physicians to provide families with a definitive prognosis and accurate information about the risk of recurrence in future pregnancies.