Understanding Marfan Syndrome
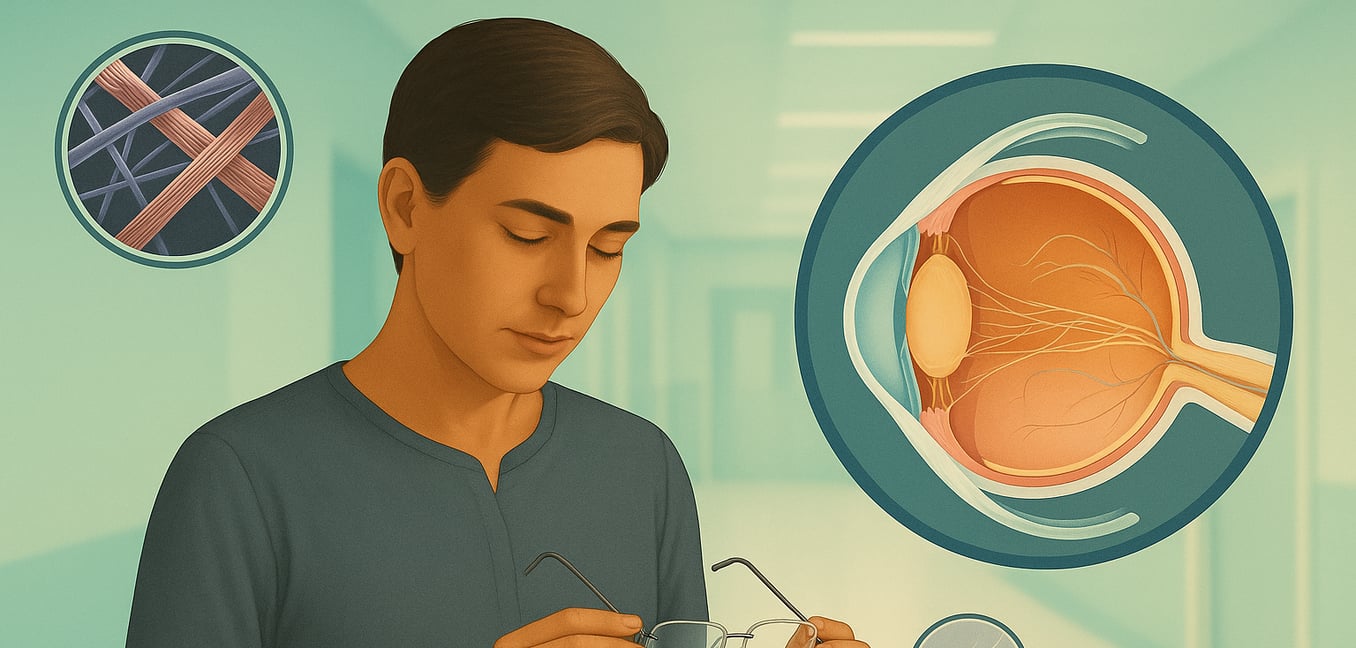
Marfan syndrome is a genetic disorder that impacts the body's connective tissue. This tissue functions as a structural "glue," providing strength and elasticity to organs, blood vessels, bones, and joints. The condition is caused by a mutation in the FBN1 gene, which is responsible for producing fibrillin-1, a crucial protein for healthy connective tissue. Because this tissue is present throughout the body, Marfan syndrome can affect multiple systems, with the most significant impacts seen in the heart, skeleton, and eyes.
The physical signs of Marfan syndrome often become more apparent with age. Common skeletal features include a tall, slender build with unusually long arms, legs, and fingers (arachnodactyly). Other indicators can be a curved spine (scoliosis), highly flexible joints, and a chest that either sinks inward (pectus excavatum) or protrudes outward (pectus carinatum). While cardiovascular monitoring is the most critical aspect of managing the condition, the effects on vision are often among the earliest and most distinct signs, prompting diagnosis and requiring specialized lifelong care.
How Marfan Syndrome Directly Affects Eye Structures
The eye is a complex organ that depends on strong, flexible connective tissue to maintain its precise shape and function. The genetic defect in fibrillin-1 weakens these essential components, leading to a range of predictable and serious vision problems.
Dislocated Lens (Ectopia Lentis)
One of the hallmark signs of Marfan syndrome is ectopia lentis, or a dislocated lens. The eye's natural lens is held in place by a network of tiny fibers called ciliary zonules. These zonules, rich in fibrillin-1, become weak and stretched in Marfan syndrome, causing the lens to shift from its central position. This displacement can range from a slight wobble to a complete dislocation.
This instability severely disrupts the eye's ability to focus light, leading to significant vision problems. Common effects include severe nearsightedness and high degrees of astigmatism, resulting in blurry or distorted vision. If the edge of the displaced lens drifts into the line of sight, it can cause double vision in a single eye, a condition known as monocular diplopia. In children, the poor focus caused by ectopia lentis can lead to amblyopia ("lazy eye") if not addressed promptly.
A severely dislocated lens can also cause urgent medical issues. If it moves forward, it can block fluid drainage and trigger a sudden, painful spike in eye pressure (acute glaucoma). If it falls backward, it can cause chronic inflammation or pull on the retina, increasing the risk of a tear or detachment.
Changes in Eye Shape and Focus
Beyond the dramatic issue of a dislocated lens, Marfan syndrome alters the fundamental shape of the eye, leading to significant refractive errors. The most common are high nearsightedness (myopia) and astigmatism.
Nearsightedness in Marfan syndrome is typically caused by the eyeball growing longer than average from front to back, a condition called increased axial length. The sclera, the white outer wall of the eye, is weaker due to faulty connective tissue. Like an overinflated balloon, the internal pressure of the eye can cause the sclera to stretch over time. This elongation means that light focuses in front of the retina instead of directly on it, making distant objects appear blurry.
Astigmatism, which causes distorted vision at all distances, is also very common and often complex. It occurs when the eye's focusing surfaces are not perfectly round. In Marfan syndrome, this can be caused by two factors: the cornea (the clear front surface) is often flatter and thinner than normal, and the lens itself may be tilted or irregularly shaped due to the weak zonules holding it in place. This combination creates a complex refractive error that can be difficult to fully correct with standard eyeglasses.
Increased Risk for Other Serious Conditions
The structural weaknesses caused by Marfan syndrome also place individuals at a much higher risk for other serious eye conditions, often at a younger age than the general population.
Early-onset glaucoma is a major concern. Glaucoma damages the optic nerve, typically due to high pressure inside the eye, and can cause permanent loss of peripheral vision. In addition to the risk of acute glaucoma from a dislocated lens, people with Marfan syndrome are more susceptible to open-angle glaucoma, where the eye's drainage channels become less efficient over time, possibly due to the same connective tissue abnormalities.
Premature cataracts are also common, sometimes developing as early as a person's 40s or 50s. A cataract is a clouding of the eye's naturally clear lens, which makes vision appear foggy or dim. This early onset is thought to be related to the chronic mechanical stress placed on the lens by weak zonules.
Finally, retinal detachment is a medical emergency that poses a significant threat. The stretching of the eyeball in high myopia makes the retina—the light-sensitive tissue at the back of the eye—thinner and more fragile, increasing the likelihood of tears or detachment.
Management and the Importance of Eye Care
Managing the visual impact of Marfan syndrome requires proactive and specialized ophthalmologic care. Because the eye structures are inherently fragile, regular monitoring is essential to detect changes early and prevent irreversible vision loss. Comprehensive annual eye exams are a cornerstone of care.
For many, vision can be managed effectively with non-surgical solutions. Specialized glasses or custom contact lenses are often required to correct the high degrees of nearsightedness and complex astigmatism associated with the condition.
When corrective lenses are no longer sufficient or when complications arise, surgery becomes necessary. For a significantly dislocated lens or a progressing cataract, the procedure involves removing the unstable natural lens and replacing it with a secure, artificial intraocular lens (IOL). This is a complex surgery that may require special devices, like capsular tension rings or sutures, to fix the new lens firmly in place. Other procedures, such as laser treatments or surgery to create new drainage pathways, may be needed to control glaucoma. Due to the underlying tissue fragility, any eye surgery on a person with Marfan syndrome requires careful planning by an experienced surgeon.